Summary
National survey data from 2019 indicate that among adults age ≥18 years with diabetes, 93.4% had health insurance coverage, including 88.9% of those age 18–64 years and 98.8% of those age ≥65 years. An estimated 1.56 million adults with diabetes had no health insurance coverage, including 1.43 million adults age 18–64 years and 130,000 adults age ≥65 years. Following the enactment of the Patient Protection and Affordable Care Act (ACA) in 2010, the proportion of individuals with health insurance in the United States increased. For adults age 18–64 years with diabetes, health insurance coverage increased from 84.7% in 2009 to 90.1% in 2016, 88.9% in 2019, and 89.8% in 2021.
In 2019, for adults with diabetes age 18–64 years, Hispanic people had a lower prevalence of health insurance coverage (75.8%) compared to people who were non-Hispanic White (93.2%), non-Hispanic Black (90.5%), and non-Hispanic Asian (98.3%). The majority of adults age 18–64 years with diabetes had private insurance coverage (57.4%); other forms of insurance were Medicaid (23.9%), Medicare (16.0%), and military benefits (4.1%). Finally, the proportion of income spent on private insurance premiums was greater for those whose income was closest to the poverty level compared to those with higher income.
During 2017 through March 2020, insured adults with diabetes had greater health care utilization compared to uninsured adults with diabetes, including more often seeing a doctor in the past year and having an eye exam. In addition, insured adults age 20–64 years with diabetes more often checked their blood glucose ≥1 time per day (45%) and had their glycosylated hemoglobin (A1c) checked regularly (88%) compared to their uninsured adult counterparts (18% and 54%, respectively). Finally, insured adults with diabetes had better A1c and cholesterol control compared to those without insurance.
Introduction
Historically, in the United States, the foundation for health insurance was employer-based coverage for working families. Most working-age adults obtained health insurance for themselves and their dependents as a benefit of employment (1). Individuals who served in the active-duty military for 24 continuous months, were discharged for a disability that was caused by or made worse by active-duty service, and did not receive a dishonorable discharge are eligible for military health insurance benefits through the Department of Veterans Affairs. With passage of the Social Security Amendments of 1965, Medicaid programs were established to provide care to people with lower incomes, and Medicare was established to provide care to virtually all Americans 65 years of age and older and younger people who were medically disabled or had end-stage kidney disease requiring dialysis or transplant. While people could purchase private health insurance on their own, this patchwork system left substantial numbers of Americans uninsured, including employed workers whose employers did not provide health insurance coverage and economically disadvantaged Americans whose incomes exceeded eligibility thresholds for Medicaid (2,3).
Many of these gaps in access to health insurance were addressed by the health care reform law, the Patient Protection and Affordable Care Act (ACA), enacted in March 2010. The ACA extended health insurance coverage to individuals who were not eligible for employer-sponsored health insurance coverage by offering them ACA marketplace coverage at subsidized rates. With the development of the ACA, the use of high-deductible health plans (HDHP) increased significantly as a way to limit health insurance premium growth (4). In parallel, health savings accounts (HSAs) were established to provide a way to save for medical expenses free from federal taxes. The ACA was also designed to address the needs of people with lower incomes who did not meet Medicaid eligibility requirements by expanding Medicaid eligibility to those in the next lowest income tier (5). The increasing prevalence of HDHPs offered by employers, the termination of the ACA’s individual insurance mandate in 2019, and lack of expanded Medicaid coverage in 12 states may leave substantial numbers of Americans underinsured or uninsured (6,7). Data described here update the information presented in the Diabetes in America, 3rd edition chapter Health Insurance and Diabetes (8).
Sources and Limitations of Data on Health Insurance
Information on health insurance is available from several surveys conducted in the United States that use national probability samples. Here, data from the National Health Interview Survey (NHIS) 2019 (9) are utilized to estimate health insurance coverage before the coronavirus disease of 2019 (COVID-19) pandemic. Overall trends in health insurance also include data from the NHIS conducted in 2021. The NHIS is a cross-sectional household interview survey that uses a complex sampling design and has been conducted continuously since 1957. Participants are asked detailed questions about diabetes and health insurance coverage. Diabetes is determined if participants answer “yes” to the following question: “(If female, other than during pregnancy) Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” Health insurance questions include items on type and source of coverage, reasons for no health insurance, and health care costs. Although the health insurance questions in the NHIS are comprehensive, a limitation is that the data are self-reported; however, participants were encouraged to bring their health insurance cards to the interview, and previous studies have supported the validity of self-reported insurance information (10,11,12). In addition, a considerable proportion of NHIS respondents with private insurance were unaware of private insurance premium costs (18%). Thus, estimates of the proportion of income spent on premiums or family medical care should be interpreted with caution. In 2019, the NHIS underwent a redesign that included changes to survey components, instruments, and the approach to weighting the sample to ensure national representativeness. An evaluation of select health insurance indicators demonstrated partial impacts of the changes to either the weighting approach or both instrument and weighting changes (13). Therefore, trends using data pre- and post-redesign should be interpreted with caution. Finally, an estimated 0.5% did not respond to the question on health insurance.
The National Health and Nutrition Examination Survey (NHANES) is another cross-sectional, national probability sample that has been conducted periodically since 1971 and continuously since 1999 (14). NHANES data collected from individuals for the period January 2017 through March 2020 before the start of the COVID-19 pandemic are utilized for national estimates. Participants self-reported diabetes status, health insurance coverage, and health care utilization. An advantage of the NHANES is that the survey includes a health exam in a mobile examination center where laboratory measures are also collected. Thus, the NHANES has diabetes-related clinical and laboratory information, such as blood pressure, glycosylated hemoglobin (A1c), and cholesterol levels.
The Medical Expenditure Panel Survey (MEPS) 2019 is a large-scale national survey with several components that collect information about families and individuals, their medical providers, and their employers. The MEPS began in 1996 and contains data on health care use, expenditures, sources of payment, and health insurance coverage for the U.S. civilian noninstitutionalized population (15). For the data presented herein, expected sources of payment were determined for medical services used by adults with diabetes. Similar to other national surveys, a limitation of the MEPS is that the data are self-reported; however, the medical provider component of the MEPS validates the information received during the household interview.
The National Ambulatory Medical Care Survey (NAMCS) 2018 is a national survey designed to collect information about the provision and use of ambulatory medical care services in the United States (16). These data are based on a sample of visits to non-federally-employed, office-based physicians who are primarily engaged in direct patient care. Similarly, the National Hospital Ambulatory Medical Care Survey (NHAMCS) 2018 is designed to collect data on the utilization and provision of ambulatory care services in hospital emergency departments (16). Data are collected from a national sample of general and short-stay hospitals, exclusive of Federal, military, and Veterans Administration hospitals. Both surveys are based on visits to health care providers and include information on costs and sources of payment for care. Expected sources of payment were determined for people with a diagnosis of diabetes.
The Behavioral Risk Factor Surveillance System (BRFSS) is a large, state-based, telephone-based survey conducted annually to collect data on respondents’ health-related behaviors, chronic health conditions, and use of preventive services (17). Data from 2009 and 2019 are presented. While data in the BRFSS are self-reported, an advantage of the survey is the ability to assess state-level estimates that are representative of the state’s population.
Statistical Methods
All estimates from national surveys are weighted to produce estimates that are nationally representative of the noninstitutionalized U.S. population. For the bar charts and tables presented herein, 95% confidence intervals and weighted standard errors are provided for the estimates, respectively. Statistical differences in estimates are based on 95% confidence intervals. The relative standard error (RSE = [SE/estimate]*100) is provided in tables and figures for estimates that are likely unreliable due to sample size. Estimates with RSEs >50% are censored.
Health Insurance Coverage and Types of Coverage by Demographics
Prevalence of Health Insurance Coverage by Age
Data from the NHIS 2019 indicate that 93.4% of all adults with diabetes had some type of health insurance coverage compared to 87.8% of adults without diabetes (Figure 1). For adults with diabetes age 18–64 years, 88.9% had health insurance coverage compared to 85.2% without diabetes. The difference in health insurance coverage by diabetes status decreased with increasing age. The prevalence of health insurance coverage for adults age ≥65 years (and eligible for Medicare) was similar regardless of diabetes status (98.8% for those with diabetes and 99.0% for those without diabetes).
FIGURE 1.
Prevalence of Health Insurance Coverage, by Diabetes Status and Age, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Prevalence of Health Insurance Coverage by Sex
Among adults age 18–64 years, more men with diabetes had health insurance coverage (89.0%) compared to men without diabetes (83.6%); the prevalence of health insurance was similar for women by diabetes status (88.7% with diabetes and 86.0% without diabetes) (Table 1).
TABLE 1.
Prevalence of Health Insurance Coverage Among Adults Age 18–64 Years, by Demographic Characteristics, U.S., 2019
Among adults age 18–64 years with diabetes, the prevalence of health insurance was similar for men and women (89.0%) (Table 1). For those without diabetes, more women had health insurance coverage compared to men (86.0% vs. 83.6%).
Prevalence of Health Insurance Coverage by Race and Ethnicity
For adults age 18–64 years with diabetes, the prevalence of health insurance coverage was higher for non-Hispanic White and non-Hispanic Asian persons compared to their counterparts without diabetes. Prevalence was similar by diabetes status for non-Hispanic Black, Hispanic, and Mexican American persons (Figure 2, Table 1). Additionally, there were no significant differences by diabetes status among groups of persons according to their race/ethnicity groups age ≥65 years (data not shown).
FIGURE 2.
Prevalence of Health Insurance Coverage for Adults Age 18–64 Years, by Diabetes Status and Race/Ethnicity, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
For adults age 18–64 years with diabetes, the prevalence of health insurance for non-Hispanic White people and non-Hispanic Black people was similar, with 93.2% and 90.5% having health insurance coverage, respectively (Figure 2, Table 1). Hispanic adults with diabetes had the lowest prevalence of insurance coverage (75.8%), and non-Hispanic Asian people with diabetes had the highest prevalence (98.3%). Among adults age ≥65 years with diabetes, nearly all non-Hispanic White and non-Hispanic Black people had health insurance coverage (>99.0%), with slightly lower prevalences of insurance coverage for Hispanic (94.0%) and non-Hispanic Asian (94.5%) people (data not shown).
For adults age 18–64 years without diabetes, 89.6% of non-Hispanic White, 85.3% of non-Hispanic Black, 69.3% of Hispanic, and 92.6% of non-Hispanic Asian people had health insurance coverage (Figure 2, Table 1). For adults age ≥65 years without diabetes, coverage was similar by race/ethnicity for non-Hispanic White, non-Hispanic Black, and non-Hispanic Asian people (>99.0% for all) but significantly lower for Hispanic people (91.7%) (data not shown).
Prevalence of Health Insurance Coverage by Education and Poverty Levels
Adults age 18–64 years with diabetes who had a high school education or who had less than a high school education were more likely to have health insurance than their counterparts without diabetes (89.9% vs. 80.7% for high school graduates and 81.6% vs. 66.4% for those with less than high school education), but insurance coverage was similar by diabetes status for higher education levels (Table 1). Adults age 18–64 years with diabetes who had a poverty income ratio (PIR, defined as family income divided by the federal poverty threshold) <1.0 or 1.0–<2.0 more often had health insurance compared to those without diabetes (81.8% vs. 72.8% for PIR <1.0 and 82.8% vs. 71.7% for PIR 1.0–<2.0, respectively). The magnitude of the difference in health insurance coverage by diabetes status decreased as PIR increased, but coverage remained higher for those with diabetes compared to those without diabetes even at the highest category of PIR (98.0% vs. 95.3% for PIR ≥4.0).
Among adults age 18–64 years with diabetes, the prevalence of health insurance coverage generally increased with higher levels of education, ranging from 81.6% for those with less than a high school education to 96.5% for those with a master’s or professional degree. Similarly, the prevalence of health insurance coverage increased with increasing PIR, ranging from 81.8% for those with PIR <1.0 to 98.0% for those with PIR ≥4.0. Health insurance coverage was similar by marital status.
Similar to those with diabetes, the prevalence of health insurance coverage increased with higher levels of education and PIR for adults without diabetes.
Prevalence of Health Insurance Coverage by Duration of Diabetes
Among adults age 18–64 years with diabetes, the prevalence of health insurance coverage increased with duration of diabetes and ranged from 81.4% for adults with newly diagnosed diabetes (<1 year) to 91.9% for adults who had been diagnosed for ≥20 years (Table 2).
TABLE 2.
Prevalence of Health Insurance Coverage Among Adults Age 18–64 Years With Diabetes, by Duration of Diabetes, U.S., 2019
Types of Health Insurance Coverage
Types of health insurance coverage were not mutually exclusive. More adults age 18–64 years with diabetes had Medicare and Medicaid/other public insurance coverage compared to those without diabetes (16.0% vs. 3.1% and 23.9% vs. 13.6% for those with and without diabetes, respectively) (Figure 3). Accordingly, fewer people with diabetes had private insurance coverage (57.4%) compared to those without diabetes (68.2%). A similar proportion of people with and without diabetes had coverage through military benefits (4.1% and 3.8%, respectively). Among adults age ≥65 years, prevalence of Medicare coverage was similar by diabetes status (95.3% with diabetes and 93.2% without diabetes), but fewer adults age ≥65 years with diabetes had private insurance compared to those without diabetes (44.2% vs. 51.6%). Medicaid/other public insurance (14.6% vs. 7.8%) and military benefits (14.2% vs. 10.3%) were higher for people with diabetes compared to those without diabetes. These differences by diabetes status remained when prevalence of health insurance type was stratified by race/ethnicity (Appendix A1).
FIGURE 3.
Types of Health Insurance Coverage Among Adults, by Diabetes Status and Age, U.S., 2019. Types of health insurance are not mutually exclusive. Data are self-reported. Error bars represent 95% confidence intervals.
For adults age 18–64 years with diabetes, the majority had private insurance (57.4%) followed, in descending order, by Medicaid/other public insurance (23.9%), Medicare coverage (16.0%), and military benefits (4.1%) (Figure 3). Compared to non-Hispanic White people, non-Hispanic Black people had a higher prevalence of Medicare (24.2%) and Medicaid/other public insurance (32.6%) and a lower prevalence of private insurance (45.2%) (vs. 16.3%, 18.3%, and 66.9% for non-Hispanic White people, respectively); and Hispanic people had a lower prevalence of Medicare (9.3%) and private insurance (41.8%) and a higher prevalence of Medicaid/other public insurance (29.9%) (vs. 16.3%, 66.9%, and 18.3% for non-Hispanic White people, respectively) (Appendix A1). Among adults ≥65 years with diabetes, the vast majority had Medicare (95.3%), while 44.2% also had private insurance, 14.6% had Medicaid/other public coverage, and 14.2% had military benefits.
Among adults age 18–64 years without diabetes, the majority had private insurance (68.2%) followed, in descending order, by Medicaid/other public insurance (13.6%), military benefits (3.8%), and Medicare coverage (3.1%). The prevalence of Medicare was similar by race/ethnicity, but non-Hispanic Black and Hispanic people had a lower prevalence of private insurance and a higher prevalence of Medicaid/other public insurance compared to non-Hispanic White people (Appendix A1). For adults age ≥65 years without diabetes, 93.2% had Medicare coverage, 51.6% had private insurance, and 8%–10% had Medicaid/other public insurance or military benefits.
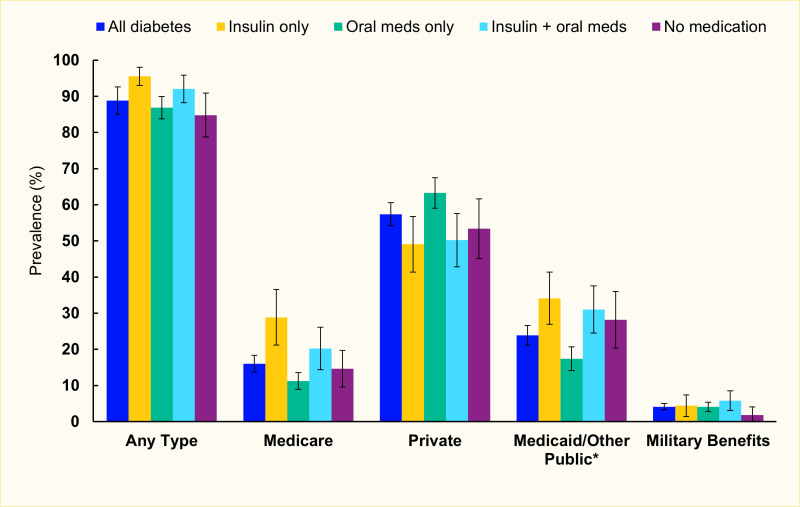
Prevalence and Types of Health Insurance Coverage by Glycemic Medication Use
The prevalence of any health insurance coverage among adults with diabetes age 18–64 years was highest for people taking insulin as their only antihyperglycemic medication (95.5%) and lowest for those not taking any medication (84.8%) (Figure 4). The prevalence of Medicare coverage was highest for those taking insulin only (28.9%) and lowest for those taking oral medication only (11.3%). The prevalence of private insurance was highest for those taking oral medication only (63.3%) and lowest for those taking insulin only (49.1%).
For adults age ≥65 years with diabetes, there was no difference in any health insurance coverage or type of health insurance coverage by medication use (data not shown).
Number of Sources of Health Insurance Coverage
For insured adults age 18–64 years, those with diabetes were more likely to have two sources of insurance (13.0%) compared to those without diabetes (3.9%) (Figure 5). Fewer adults age ≥65 years with diabetes had only one source of health insurance compared to those without diabetes (34.9% vs. 39.4%).
For insured adults with diabetes age 18–64 years, the majority had one source of health insurance (86.5%), and 13.0% had two health insurance sources. Among insured adults with diabetes age ≥65 years, the majority had two health insurance sources (59.9%). About one-third had one health insurance source (34.9%), and 5.2% had three or more sources.
Among insured adults age 18–64 years without diabetes, 96.0% had one source of health insurance, and 3.9% had two sources. For insured adults age ≥65 years without diabetes, the majority had two sources of insurance (56.9%), followed by 39.4% having one source and 3.7% having three or more sources.
Prevalence of Private Health Insurance
For adults with diabetes, private health insurance coverage was less frequent among all adults combined and less frequent in all individual age groups compared to those without diabetes (51.4% vs. 65.1% overall, 45.9% vs. 64.0% at age 18–34 years, 54.9% vs. 70.2% at age 35–49 years, 59.6% vs. 71.9% at age 50–64 years, and 44.2% vs. 51.6% at age ≥65 years) (Figure 6).
FIGURE 6.
Prevalence of Private Health Insurance Coverage Among Adults, by Diabetes Status and Age, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
In 2019, among adults with diabetes age 18–64 years with private insurance, nearly one-third had an HDHP, including 10.7% with HSAs and 21.5% without HSAs (Table 3). HSAs are a type of savings account for people with HDHPs to save for qualified medical expenses on a pre-tax basis. The prevalence of an HDHP was lower for adults with diabetes age ≥65 years (11% in total, including 1.4% with HSAs and 9.5% without HSAs). Results were similar for those without diabetes.
TABLE 3.
Prevalence of a High-Deductible Health Plan Among Adults With Private Health Insurance, by Diabetes Status and Age, U.S., 2019
Sources of Private Health Insurance
For adults age 18–64 years with private insurance, the vast majority of private health insurance plans were obtained through the employer or workplace compared to other sources, regardless of diabetes status (82.1% and 87.9% for those with and without diabetes, respectively) (Figure 7). The prevalence of purchasing a private plan through a health insurance exchange or marketplace was 10.6% for those with diabetes and 6.9% for those without diabetes. The prevalence of purchasing a non-employer sponsored private plan directly was 5.1% for adults with diabetes and 4.2% for adults without diabetes.
FIGURE 7.
Sources of Private Health Insurance Among Adults Age 18–64 Years, by Diabetes Status, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Coverage for Specific Aspects of Health Care
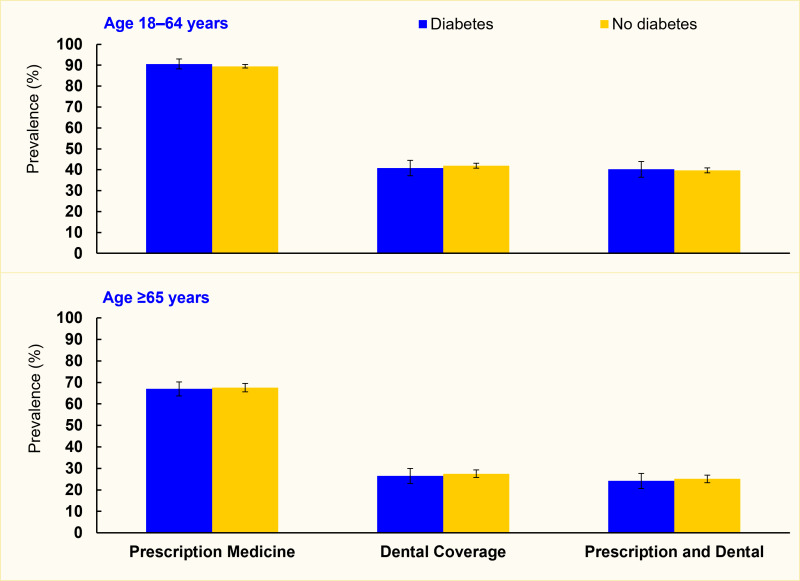
Prescription Medication and Dental Coverage
For adults age 18–64 years with private health insurance, there were no differences between persons with and without diabetes in the prevalences of prescription medication coverage and dental coverage (Figure 8). The prevalence of prescription coverage was 90.6% for people with diabetes and 89.5% for people without diabetes. Dental coverage prevalence was 40.8% for those with diabetes and 41.9% for those without diabetes. Forty percent of people with diabetes and 39.7% of those without diabetes had both prescription and dental coverage.
FIGURE 8.
Prevalence of Prescription Medication and Dental Coverage Through a Private Health Insurance Plan Among Adults, by Diabetes Status and Age, U.S., 2019. Data are self-reported. Error bar represent 95% confidence intervals.
For privately insured adults age ≥65 years with diabetes, 67.0% had prescription coverage, 26.5% had dental coverage, and 24.2% had both. The prevalences were 67.6%, 27.5%, and 25.1%, respectively, for those without diabetes.
Medicare Parts A–D
In 2019, among Medicare beneficiaries age ≥65 years with diabetes, 44.1% had both Part A (Hospital Insurance) and Part B (Medical Insurance) only (Figure 9). An additional 49.9% had Parts A, B, and D (prescription drug plan). Few had Part A only (4.9%) or Part B only (1.2%). For Medicare beneficiaries with diabetes, 32.2% had a Medicare Advantage plan (not mutually exclusive to the distribution of Medicare parts), which provides traditional Medicare benefits through a private company and often provides additional benefits like vision, hearing, and dental care not covered by traditional Medicare (data not shown). Between 2010 and 2019, the prevalence of Medicare Advantage increased from 18.7% to 32.2% among people with diabetes (Appendix A2). About 50% of Medicare beneficiaries with diabetes had Part D coverage regardless of glycemic medication use status or type of glycemic medication used (insulin only, oral only, both) (data not shown).
FIGURE 9.
Prevalence of Medicare Parts Among Adults Age ≥65 Years, by Diabetes Status, U.S., 2019. Medicare Part A: Hospital Insurance; Part B: Medical Insurance; Part D: prescription medication coverage. Data are self-reported.
The prevalence of Medicare parts was similar among adults age ≥65 years without diabetes, including 48.2% who had both Part A and Part B only, 45.2% who had Parts A, B, and D, and 32.4% who had Medicare Advantage. Similar to those with diabetes, the prevalence of Medicare Advantage increased from 18.1% in 2010 to 32.4% in 2019 for those without diabetes (Appendix A3).
Additional Health Insurance Coverage
Combinations of Health Insurance Plans Among People With Medicare Coverage
For adults with diabetes age 18–64 years with Medicare coverage, 34.4% had Medicare as their only source of insurance, but over one-third also had Medicaid coverage (37.8%); 19.6% also had private insurance coverage, and a smaller proportion also had military benefits (5.0%) (Figure 10). For adults with diabetes age ≥65 years with Medicare, 32.9% had only Medicare coverage, and 39.6% also had private health insurance. Fewer people had Medicaid (12.3%) or military benefits (9.9%) in addition to their Medicare coverage.
FIGURE 10.
Prevalence of Combinations of Health Insurance Plan(s) Among Adults With Diabetes and Medicare, by Age, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Combinations of Health Insurance Plans Among People With Private Insurance
Among adults with diabetes age 18–64 years who reported having private insurance, the vast majority had only private coverage (91.4%), but 5.5% also had Medicare coverage (Figure 11). For adults with diabetes age ≥65 years with private insurance, few had private insurance as their only source of coverage (2.9%). Most older adults with private insurance also had Medicare coverage (85.3%), and 11.0% had private insurance plus two additional plans.
FIGURE 11.
Prevalence of Combinations of Health Insurance Plan(s) Among Adults With Diabetes and Private Insurance, by Age, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Trends in Health Insurance Coverage
Health insurance coverage increased significantly for adults with diabetes after the ACA was enacted in 2010 to improve access, affordability, and quality of medical care in the United States. Many provisions took effect in 2014 (18). For adults age 18–64 years with diabetes, health insurance coverage increased from 84.7% in 2009 to 90.1% in 2016, 88.9% in 2019 (pre-COVID-19), and 89.8% in 2021 (during the COVID-19 pandemic) (Figure 12) (19). Similarly, the prevalence of health insurance coverage for adults age 18–64 years without diabetes changed from 78.3% in 2009 to 88.3% in 2016, 85.2% in 2019, and 87.2% in 2021. While those with diabetes had higher prevalence of coverage, during this period, the magnitude of the difference in health insurance coverage by diabetes status decreased. Future analyses can determine whether the plateau in coverage between 2016 and 2021 will continue. While health insurance coverage steadily increased between 2010 and 2016 due to the ACA, the plateau between 2016 and 2021 may be attributed to repeals of the individual mandate, limits placed on outreach and opportunities for enrollment in marketplace plans, reductions in subsidies for marketplace plans, changing rules to allow HDHPs with fewer benefits, implementing the “public charge” rule, which may have led to a cooling-off effect for public insurance coverage among people who have recently immigrated, and state policies that made it harder to enroll or stay enrolled in Medicaid (19,20,21,22).
FIGURE 12.
Trends in Health Insurance Coverage Among Adults Age 18–64 Years, by Diabetes Status, U.S., 2009–2021. Data are self-reported. Error bars represent 95% confidence intervals.
Among adults age 18–64 years, the prevalence of health insurance in 2019 continued to be higher for those with diabetes compared to those without diabetes, but the magnitude of the difference in health insurance coverage between those with and without diabetes decreased between 2009 and 2021 for non-Hispanic Black, Hispanic, Mexican American, and non-Hispanic Asian people (Figure 13, Appendix A4). This relationship was also observed for those whose highest level of education was a high school or an associate degree, those with a PIR <1.0, and those divorced or separated. There were few changes in the type of health insurance coverage between 2009 and 2021 among adults age 18–64 years, with the majority having private insurance, regardless of diabetes status (data not shown). Figure 14 shows the percentage change in health insurance coverage between 2009 and 2019 by state among adults with and without diabetes. Regardless of diabetes status, health insurance coverage increased between 2009 and 2021 by ≥5.0% in Louisiana, Arkansas, Kentucky, West Virginia, New Mexico, Oregon, and Alaska.
FIGURE 13.
Prevalence of Health Insurance Coverage Among Adults Age 18–64 Years, by Diabetes Status and Race/Ethnicity, U.S., 2009 and 2021. Data are self-reported. Error bars represent 95% confidence intervals.
FIGURE 14.
Difference in Health Insurance Coverage Before and After the ACA, by Diabetes Status and State, U.S., 2009 and 2019. Differences are statistically significant except where noted. Data are self-reported. ACA, Patient Protection and Affordable Care Act. (more...)
As part of the ACA, insurers cannot deny coverage to people with preexisting conditions, including diabetes, and must provide affordable premiums; these regulations became effective January 1, 2014 (18). Among a privately insured population age 20–59 years, a study using data from the Clinformatics Data Mart Database found a 4% lower prevalence rate of type 1 diabetes among insured individuals before the preexisting condition exclusion mandate (2005–2013) and an 11% increase in prevalence rate between 2014 and 2016 after the mandate went into effect (23). There was a significant decrease in type 2 diabetes prevalence before the mandate and an increase in type 2 diabetes prevalence afterwards for the 40–49 and 50–59 years age groups. Thus, more people with diabetes appeared to obtain private insurance after the implementation of the preexisting condition allowance mandate. In our analysis, prevalence of private health insurance remained steady between 2009 and 2019 for adults age 18–64 years with diabetes (58.3% in 2009 vs. 57.4% in 2019, data not shown), although the prevalence of any type of health insurance coverage increased (from 84.7% in 2009 to 88.9% in 2019).
Another provision of the ACA called for the expansion of Medicaid eligibility to provide insurance coverage for more people with lower incomes (24). Under the expansion, Medicaid eligibility would extend to include adults 18–64 years with incomes up to and including 138% of the federal poverty level in all 50 states. However, in 2012, the Supreme Court ruled that the states could not be forced to expand their Medicaid programs. In 2014, Medicaid was expanded in 26 states, and by the end of 2021, Medicaid had been expanded in 38 states. Data from the BRFSS 2009 and 2019 show that the prevalence of health insurance coverage among adults with diabetes increased more for states with Medicaid expansion compared to those without expansion (Figure 15). The increase in health insurance coverage was largest among those with a household income <$20,000, regardless of whether residence was in a Medicaid expansion state or not. In addition, insurance coverage decreased slightly between 2009 and 2019 for individuals with household incomes $35,000–$75,000 in states without Medicaid expansion. In a study conducted in 644 counties across the southern and eastern United States where diabetes prevalence is ≥11%, Medicaid expansion was associated with a nearly 50% reduction in rates of uninsurance (25). Among adults with diagnosed diabetes who participated in the BRFSS 2011–2016, there were significant improvements in self-reported access to health care, diabetes management, and general health status for those residing in states with Medicaid expansion compared to those residing in states without Medicaid expansion (26). In the Medicaid Drug Spending and Utilization 2012–2017 data set, use of noninsulin antihyperglycemic therapies increased among low-income adults in both Medicaid expansion and non-expansion states, with a significantly greater increase in therapies observed in expansion states (27). Data from the BRFSS showed that Medicaid expansion policies were significantly associated with an increase in rate of dilated eye exams among adults with diabetes within the first 2 years of implementation, but the rate plateaued beyond this time period (28). Lastly, data from federally qualified health centers showed that Medicaid expansion was associated with sustained increased in insurance coverage and improved glucose control over 5 years among Black and Hispanic populations (29).
FIGURE 15.
Percent Change in Health Insurance Coverage Between 2009 and 2019 Among Adults With Diabetes, by States With and Without Medicaid Expansion and Household Income, U.S., BRFSS. Data are self-reported.
Health Insurance and Diabetes Care
Health Insurance and Quality of Diabetes Care
Management of diabetes and its complications is affected by access to health care, health care utilization, access to medical supplies and prescription medications, and education on how to manage diabetes. Detailed analyses related to the multiple factors associated with the quality of care for diabetes are out of the scope of this report. An overview of health insurance and its association with diabetes care is provided in this section.
Data from the United States Diabetes Surveillance System, a Centers for Disease Control and Prevention (CDC) interactive web application, estimates that 83.8% of adults age ≥18 years with diabetes took a diabetes medication in 2019 (30). These adults used various combinations of insulin, injectable and oral glucose-lowering medications, lipid-lowering medications, and antihypertensive medications. Data from the NHANES 2017–March 2020 among adults age 20–64 years with diabetes showed that self-reported current use of insulin as the only antihyperglycemic medication was higher among those with health insurance compared to those without health insurance (12.7% vs. 2.5%) (Table 4). Frequencies of use of antihypertensive and antilipidemic medications were also higher for those with health insurance compared to those without insurance (57.5% vs. 35.6% and 53.2% vs. 28.8%, respectively).
TABLE 4.
Prevalence of Medication Use Among Adults Age 20–64 Years With Diabetes, by Health Insurance Status, U.S., 2017–March 2020
Studies have demonstrated that diabetes self-management education and support increases patients’ success in managing their diabetes (31,32). Data from the NHANES 2017–March 2020 show that more adults age 20–64 years with health insurance regularly checked their blood glucose at least once per day (45.2%) compared to those without insurance (18.2%) (Table 5). Diabetes self-management requires knowledge and resources, both of which are impacted by types of health insurance coverage. One study showed that 20 states did not require Medicaid to cover diabetes self-management education and training (33).
TABLE 5.
Prevalence of Quality of Care and Health Care Utilization Among Adults Age 20–64 Years With Diabetes, by Health Insurance Status, U.S., 2017–March 2020
Health Insurance and Health Care Utilization
Data from the NHANES 2017–March 2020 showed that among adults age 20–64 years with diabetes, 95.9% with health insurance reported having a routine place to go for health care compared to 62.0% of those without health insurance (Table 5). This association remained when estimates were stratified by race/ethnicity (Appendix A5). In addition, 82.1% of adults with diabetes and health insurance reported having one doctor or other health professional for diabetes care compared to 47.3% of adults with diabetes but without health insurance. Insured adults with diabetes were more likely to report having their A1c tested (87.9%) and having dilated eye exams (63.3%) in the past year compared to their uninsured counterparts (54.2% and 33.7%, respectively). A previous study from the NHANES 2009–2012 showed that adults age 18–64 years with diabetes who had Medicaid or private insurance were more likely to have a foot exam or eye exam in the past year compared to those without insurance (34).
Data from the National Survey of Children’s Health 2016–2019 found that children age 0–17 years with diabetes and health insurance coverage gaps were significantly less likely to visit a specialist in the past year compared to children with diabetes and continuous private insurance (35).
Data from the NHIS 2019 show that 6.9% of insured adults age 18–64 years with diabetes delayed medical care due to cost in the past year compared to 32.1% of uninsured adults with diabetes (Table 6). In addition, 6.1% of persons with diabetes and health insurance reported that they needed medical care but delayed it due to cost compared to 30.2% of those without health insurance. Similar associations were seen among older adults age ≥65 years, with even larger differences.
TABLE 6.
Prevalence of Delaying Medical Care Among Adults With Diabetes, by Health Insurance Status and Age, U.S., 2019
Health Insurance and Diabetes Management
Data from the NHANES 2017–March 2020 show that A1c and cholesterol management were better for insured adults age 20–64 years with diabetes compared to those who were uninsured (Table 7). A greater proportion of insured adults with diabetes achieved an A1c <8.0% (<64 mmol/mol) or A1c <9.0% (<75 mmol/mol) (72.0% and 85.0% vs. 53.6% and 61.9% for insured and uninsured, respectively). Among adults age 20–64 years with diabetes, 55.3% with health insurance achieved low-density lipoprotein (LDL) cholesterol <100 mg/dL (<2.59 mmol/L) versus 27.7% for uninsured, and 53.6% were taking statin medications versus 25.5% for uninsured. There were no significant differences in achieving blood pressure goals by insurance status among adults age 20–64 years with diabetes. Diabetes management by insurance status and race/ethnicity is shown in Appendix A5.
TABLE 7.
Prevalence of Diabetes Management Among Adults Age 20–64 Years With Diabetes, by Health Insurance Status, U.S., 2017–March 2020
Health Insurance, Morbidity, and Mortality
Data from the NHANES 2017–March 2020 show that among adults age 20–64 years with diabetes, the prevalence of self-reported hypertension or hyperlipidemia was higher for those with health insurance than those without insurance (Table 8). This may reflect a higher prevalence of health insurance among persons with these conditions or greater health care utilization and likelihood of diagnosis among those with insurance. Among adults age 20–64 years with diabetes, the prevalences of obesity and history of cardiovascular disease, stroke, retinopathy, or renal disease were similar by insurance status.
TABLE 8.
Prevalence of Morbidity Among Adults Age 20–64 Years With Diabetes, by Health Insurance Status, U.S., 2017–March 2020
Other studies have assessed morbidity and mortality by health insurance status among adults with diabetes. Cross-sectional data from the NHIS 2006–2016 showed that among adults age 55–74 years, Medicare eligibility was associated with a reduction in functional limitations due to diabetes, which demonstrates that expanded health insurance coverage may improve health outcomes (36). A U.S. population-based study found a significant increase in diabetic ketoacidosis and hyperglycemic hyperosmolar state among adults in the emergency department and inpatient settings between 2006 and 2014, and this increasing trend was more prominent for adults with Medicare or Medicaid compared to those with private insurance (37). A pooled cross-sectional study from the National Inpatient Sample 2009–2015 showed that patients with diabetes covered by Medicaid or who were uninsured were more likely to die during a diabetes-related hospitalization compared to those who were privately insured (38).
Health Insurance and Technology to Manage Diabetes
Over the past several decades, many technological advances have been made in the medical management of diabetes. These include Bluetooth-enabled glucose monitors, continuous glucose monitoring systems (CGMs), mHealth apps, smart pens that track insulin administration, and insulin pumps (39).
Among youth (age <18 years) with type 1 diabetes in the Type 1 Diabetes Exchange, insulin pump use and CGM use increased from 57.3% to 64.9% and 5.9% to 30.1%, respectively, between 2010–2012 and 2016–2018 (40). This finding may suggest more widespread coverage of CGM as a tool to manage diabetes.
In a retrospective cohort study of youth with type 1 diabetes and public insurance (Medi-Cal/Medicaid, Medicare, or California Children’s Services) attending the Stanford University Children’s Diabetes Clinic, use of CGM was associated with improved A1c levels at the next visit (A1c reduction of 0.3%) but only with uninterrupted CGM use (41). Nearly two-thirds of interruptions in CGM use were due to gaps in insurance and were associated with increased A1c levels.
Among youth participating in the T1D Exchange Registry, insurance coverage that included more generous coverage for insulin pumps, CGM, test strips, and other medical supplies was positively associated with insulin pump and CGM use, and the use of those devices was associated with fewer adverse outcomes (42). The study suggested that disparities in adverse diabetes outcomes may be mitigated by access to and use of technology.
While it has been established that CGM use among people with type 1 diabetes improves short-term glycemic management, use of CGM among people with type 2 diabetes has also shown utility for diabetes management (43,44). Studies have demonstrated clinical utility of CGM use in type 2 diabetes with intense or moderately intense insulin use (45,46,47,48). These studies have shown reductions in A1c and reduced glycemic variability, as well as reductions in acute diabetes-related events and inpatient hospitalizations, when people with type 2 diabetes use CGM versus standard self-monitoring of blood glucose.
Economic Aspects of Health Insurance Coverage
Out-of-Pocket Costs
A study using data from MEPS among adults age 18–64 years with diabetes found that total per-person out-of-pocket costs decreased by 4.3% from 2001 to 2017 (49). High out-of-pocket cost rates (percentage of households with out-of-pocket health care spending >10% of their family income) declined most notably among those with public or no insurance and those with low incomes. Compared to those with private insurance, those with public or no insurance had higher high out-of-pocket cost rates in the early years but had lower rates from 2009 to 2017. This finding may indicate reduced out-of-pocket payments or decreases in health care use. Future research is warranted to explore the contributing factors of these changes. While high out-of-pocket cost rates declined regardless of insulin use, the rate was significantly higher among people who used insulin.
Among Medicare beneficiaries age ≥65 years with diabetes, a study from the Medicare Current Beneficiary Survey found that the prevalence of high out-of-pocket cost burden, defined as out-of-pocket costs >10% or >20% of household income, was greatest for those in the <25% or 25%–50% household income quartiles (50). In addition, beneficiaries with diabetes had significantly higher out-of-pocket costs and were more likely to have high out-of-pocket cost burden compared to those without diabetes.
Source of Payment for Medical Services
Data from the MEPS 2019 indicate that among adults age 18–64 years with diabetes, the predominant source of payment for medical care expenses for total services (all office-based visits, emergency room visits, inpatient services, dental visits) was private insurance (51.4%); 19.1% of services were paid by Medicare, 16.2% were paid by Medicaid, 8.5% were paid out-of-pocket, and the remaining 4.8% were paid by other sources (Table 9). A similar distribution was seen for all office-based visits. For emergency room visits, 46.2% were paid by private health insurance, with 17% and 19% of emergency room visits paid by Medicare and Medicaid, respectively. The majority of dental visits were paid by private insurance (46.9%) or out-of-pocket (39.0%).
TABLE 9.
Percent Distribution of Payment for Medical Care Expenses for Adults With Diabetes, by Source of Payment and Age, U.S., 2019
For adults age ≥65 years with diabetes, the majority of total services were paid by Medicare (62.5%), with 16.1% paid by private insurance and 8.5% paid out-of-pocket (Table 9). Payment sources were distributed similarly for all office-based visits. A large majority of emergency room visits were paid by Medicare (73.2%), and most dental visits were paid out-of-pocket (53.9%).
Source of Payment for Health Care Visits Involving Diabetes
Data from the NAMCS 2018 show that for adults age 18–64 years having ambulatory office visits with diabetes as a diagnosis, 65.6% of visits were expected to be paid by private insurance, 15.1% by Medicaid, 10.3% by Medicare, and 11.1% from other sources (Table 10). Data from the NHAMCS 2018 show that for adults age 18–64 years having emergency department visits with diabetes, 27.0% of visits were expected to be paid by private insurance, 42.2% by Medicaid, 15.9% by Medicare, and 30.2% by other sources. Multiple sources of payment for a visit could occur; thus, expected sources of payment were not mutually exclusive.
TABLE 10.
Prevalence of Expected Sources of Payment for Ambulatory Physician Office Visits and Emergency Room Visits Involving Diabetes, by Source of Payment and Age, U.S., 2018
For adults ≥65 years, 80.6% of office visits were expected to be paid by Medicare, 37.6% by private insurance, 7.6% by Medicaid, and 6.7% by other sources. For emergency department visits, 72.5% were expected to be paid by Medicare, 38.4% by private insurance, 24.4% by Medicaid, and 19.2% from other sources.
Proportion of Income Spent on Private Insurance Premiums
In the NHIS 2019 data, among adults with private insurance, the proportion of family income that adults with diabetes spent on out-of-pocket private insurance premiums was higher for people with lower PIR (Figure 16). Using median premium costs, adults age 18–64 years with diabetes who had a PIR <1.0 spent 14.9% of their income on private insurance premiums, while those with a PIR ≥4.0 spent 6.1% of their income on private insurance premiums. A similar association was shown for adults age 18–64 years without diabetes.
FIGURE 16.
Proportion of Family Income Spent on Out-Of-Pocket Private Premiums in the Past Year Among Adults, by Poverty Income Ratio, Diabetes Status, and Age, U.S., 2019. Data are self-reported using median costs for private insurance premiums. Error bars represent (more...)
An inverted U-shape relationship was seen for adults age ≥65 years with diabetes. Using median costs, the proportion of income spent on out-of-pocket insurance premiums was 9.7% for those with a PIR <1.0, 12.1% for those with PIR 1.0–<2.0, 9.4% for those with PIR 2.0–<4.0, and 4.9% for those with a PIR ≥4.0. A similar association was shown for adults age ≥65 years without diabetes.
Changes in Prescription Medication Costs
In a retrospective cross-sectional study using administrative claims data for adults with commercial, Medicare, or Medicaid insurance, the average cost of antidiabetic medications per patient per month increased by 47.5% from 2014 to 2019. This increase was disproportionately greater than the increase of 8.8% in antidiabetic medication utilization (51). Data from the MEPS during 2005–2007 and 2015–2017 indicate that the increase in spending on glucose-lowering medications was mostly associated with the increased costs for insulin and newer noninsulin medicines. The proportion paid out-of-pocket increased across all sources of payment: Medicare, Medicaid, and private insurance (52). A study that utilized the IBM® MarketScan® Commercial Claims and Encounters database found that annual out-of-pocket payments for adults with diabetes increased by 4% for bolus insulin and by 21% for basal insulin from 2005 to 2018 (53). For privately insured adults with diabetes, out-of-pocket payments for annual insulin supply increased by $100 for patients using basal-bolus insulin and $86 for those using premixed insulin between 2005 and 2018. In another MarketScan® study among adults with type 2 diabetes under fee-for-service plans, average annual payments and out-of-pocket costs for noninsulin glucose-lowering drugs increased significantly from 2005 to 2018, with increased utilization of newer classes of antidiabetic medications driving the increase in costs (54).
No Health Insurance Coverage
Number and Prevalence of People Without Health Insurance
Data from the NHIS indicate that 23.6 million adults age ≥18 years had diabetes in 2019. Applying the rates of health insurance coverage estimated in Figure 1, 1.56 million adults with diabetes had no health insurance coverage, including 1.43 million adults age 18–64 years and 130,000 adults age ≥65 years (Figure 17). For adults without diabetes, 27.8 million had no health insurance coverage, including 27.3 million adults age 18–64 years and 430,000 adults age ≥65 years (data not shown).
FIGURE 17.
Number of Adults With Diabetes (in Millions) Who Do Not Have Health Insurance Coverage, by Age, U.S., 2019. Data are self-reported.
The prevalence of having no health insurance was 6.6% for all adults with diabetes and 12.2% for adults without diabetes (Figure 18). Among adults with diabetes, 11.6% of adults age 18–34 years, 13.8% of adults age 35–49 years, and 10.1% of adults age 50–64 years had no health insurance. For people without diabetes, 17.5%, 15.2%, and 10.6% had no health insurance, respectively by age group. A small proportion of adults age ≥65 years had no health insurance, including 1.2% of people with diabetes and 1.0% of people without diabetes.
FIGURE 18.
Prevalence of Having No Health Insurance Coverage, by Diabetes Status and Age, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Length of Time Without Health Insurance
Among uninsured adults with diabetes age 18–64 years, the most had been uninsured for <1 year (39.3%); 14.1% had been uninsured for 1–2 years, 19.0% had been uninsured for 2–5 years, and 27.6% had been uninsured for ≥5 years (Figure 19).
FIGURE 19.
Length of Time Since Last Had Health Insurance Among Adults Age 18–64 Years, by Diabetes Status, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Adults age 18–64 years without diabetes had been uninsured for similar lengths of time, with 35.8% having no insurance in the past year and 23.3% having no health insurance coverage for ≥5 years.
Reasons for Not Having Health Insurance
For adults with diabetes age 18–64 years, losing a job or changing employers was the most common reason for not having health insurance in the past 3 years (41.8%) (Table 11). Almost one-third reported that they did not have coverage because they were not eligible for Medicaid, CHIP, or other public coverage. An increase in cost for coverage was reported by 14.6% of adults age 18–64 years with diabetes as the reason for not having health insurance.
TABLE 11.
Reasons for No Health Insurance Among Adults Age 18–64 Years Who Were Uninsured For <3 Years, by Diabetes Status, U.S., 2019
Reasons for lack of health insurance coverage were similar for adults without diabetes, although slightly more reported cost increases and slightly fewer reported not being eligible for public coverage as reasons for no coverage.
Family Income of People Without Insurance
Among uninsured adults age 18–64 years, the distribution by PIR was similar by diabetes status (Figure 20). Among adults age 18–64 years with diabetes who were uninsured, 29.9% had a PIR <1.0 with similar proportions having a PIR 1.0–<2.0 (35.1%) or 2.0–<4.0 (30.2%). Fewer (4.9%) had a PIR ≥4.0. The distribution of PIR for uninsured adults age 18–64 years without diabetes was 20.8% for PIR <1.0, 33.9% for PIR 1.0–<2.0, 32.5% for PIR 2.0–<4.0, and 12.9% for PIR ≥4.0.
FIGURE 20.
Distribution of Adults Age 18–64 Years Without Health Insurance, by Poverty Income Ratio and Diabetes Status, U.S., 2019. Data are self-reported. Error bars represent 95% confidence intervals.
Conclusion
In 2019, the majority of U.S. adults with diabetes had health insurance coverage. Nevertheless, an estimated 1.56 million adults with diabetes had no health insurance coverage. Since the enactment of the ACA in 2010, the prevalence of people with diabetes that have health insurance coverage has increased. However, repeals of the individual mandate, reductions in subsidies, and suboptimal expansion of Medicaid may have led to a plateau in health insurance coverage between 2016 and 2021. Health insurance coverage was less frequent among people who are Hispanic, with less education, and with less income. Insured adults with diabetes had greater health care utilization and diabetes management than uninsured adults with diabetes. Lastly, the proportion of income spent on private insurance premiums was inversely associated with PIR; families with the lowest income paid a higher portion of their income on premiums compared to families with higher income. Health insurance is important for people with diabetes to effectively manage their disease; reductions in health insurance disparities may also reduce disparities in diabetes management.
List of Abbreviations and Definitions
- A1c
glycosylated hemoglobin
- ACA
Patient Protection and Affordable Care Act
- BRFSS
Behavioral Risk Factor Surveillance System
- CGM
continuous glucose monitoring
- CHIP
Children’s Health Insurance Program
- COVID-19
coronavirus disease of 2019
- HDHP
high-deductible health plan
- HSA
health savings account
- Medicaid
Health insurance program for certain individuals and families with low incomes. It is jointly funded by the state and federal governments and is managed by the state.
- Medicare
National health insurance program administered by the U.S. federal government since 1965 that guarantees access to health insurance for Americans age ≥65 years and for younger people with disabilities, including those with end-stage renal disease.
- Medicare Advantage
Health insurance plan offered by a private company that contracts with Medicare to provide Medicare Parts A and B and most often Part D.
- MEPS
Medical Expenditure Panel Survey
- Military benefits
Includes non-enlisted civilian population who have benefits from the Veterans Health Administration, TRICARE (a Department of Defense health care program), or CHAMP-VA (coverage for a spouse or widow(er) and to the children of a veteran who are not eligible for TRICARE).
- NAMCS
National Ambulatory Medical Care Survey
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHANES
National Health and Nutrition Examination Survey
- NHIS
National Health Interview Survey
- Other public insurance
Includes state-sponsored health plan, other government plan, and CHIP.
- PIR
poverty income ratio, defined as family income divided by the federal poverty threshold
Conversions
A1c: (% x 10.93) - 23.50 = mmol/mol
Cholesterol: mg/dL x 0.0259 = mmol/L
Acknowledgment
This is an update of: Casagrande SS, Cowie CC: Health Insurance and Diabetes. Chapter 42 in Diabetes in America, 3rd ed. Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, Gregg EW, Knowler WC, Barrett-Connor E, Becker DJ, Brancati FL, Boyko EJ, Herman WH, Howard BV, Narayan KMV, Rewers M, Fradkin JE, Eds. Bethesda, MD, National Institutes of Health, NIH Pub No. 17-1468, 2018, p. 42.1–42.18
Article History
Received in final form on January 20, 2023.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.
- Kaiser Family Foundation. Timeline: History of health reform in the U.S. Kaiser Family Foundation; 2011. Accessed March 25, 2011. https://www
.kff.org/wp-content /uploads/2011 /03/5-02-13-history-of-health-reform .pdf - 2.
- Chase D, Arensmeyer J. The Affordable Care Act's impact on small business. The Commonwealth Fund; 2018. Accessed October 2018. https://www
.commonwealthfund .org/sites/default /files/2018-10 /Chase_ACA_impact_small_business_ib.pdf [PubMed: 30280862] - 3.
- Claxton G, Levitt L, Pollitz K. Pre-ACA market practices provide lessons for ACA replacement approaches. Kaiser Family Foundation; 2017. Accessed February 16, 2017. https://www
.kff.org/health-costs /issue-brief /pre-aca-market-practices-provide-lessons-for-aca-replacement-approaches/ - 4.
- Miller GE, Vistnes JP, Rohde F, Keenan PS. High-deductible health plan enrollment increased from 2006 to 2016, employer-funded accounts grew in largest firms. Health Aff (Millwood). 2018;37(8):1231-1237. doi:10.1377/hlthaff.2018.0188 [PubMed: 30080451] [CrossRef]
- 5.
- Rosenbaum S. The Patient Protection and Affordable Care Act: implications for public health policy and practice. Public Health Rep. 2011;126(1):130-135. doi:10.1177/003335491112600118 [PMC free article: PMC3001814] [PubMed: 21337939] [CrossRef]
- 6.
- Eibner C, Nowak S. Understanding the impact of the elimination of the individual mandate penalty. The Commonwealth Fund; 2018. Accessed August 9, 2018. https://www
.commonwealthfund .org/blog/2018 /understanding-impact-elimination-individual-mandate-penalty - 7.
- Garfield R, Orgera K, Damico A. The coverage gap: uninsured poor adults in states that do not expand Medicaid. Kaiser Family Foundation; 2020. Accessed January 2020. https://files
.kff.org /attachment/Issue-Brief-The-Coverage-Gap-Uninsured-Poor-Adults-in-States-that-Do-Not-Expand-Medicaid - 8.
- Casagrande SS, Cowie CC. Health Insurance and Diabetes. In: Cowie CC, Casagrande SS, Menke A, et al, eds. Diabetes in America. 3rd ed. National Institutes of Health; 2018:42.1-42.18:chap 42. Accessed December 12, 2023. https://www
.ncbi.nlm .nih.gov/books/NBK567967/ - 9.
- National Center for Health Statistics. National Health Interview Survey, 2019 NHIS. Updated April 5, 2021. https://www
.cdc.gov/nchs/nhis/2019nhis .htm - 10.
- Call KT, Davidson G, Davern M, Brown ER, Kincheloe J, Nelson JG. Accuracy in self-reported health insurance coverage among Medicaid enrollees. Inquiry. 2008;45(4):438-456. doi:10.5034/inquiryjrnl_45.04.438 [PubMed: 19209838] [CrossRef]
- 11.
- Mucci LA, Wood PA, Cohen B, Clements KM, Brawarsky P, Brooks DR. Validity of self-reported health plan information in a population-based health survey. J Public Health Manag Pract. 2006;12(6):570-577. doi:10.1097/00124784-200611000-00011 [PubMed: 17041306] [CrossRef]
- 12.
- Pascale J, Fertig AR, Call KT. Assessing the accuracy of survey reports of health insurance coverage using enrollment data. Health Serv Res. 2019;54(5):1099-1109. doi:10.1111/1475-6773.13191 [PMC free article: PMC6736923] [PubMed: 31287571] [CrossRef]
- 13.
- National Center for Health Statistics. Preliminary evaluation of the impact of the 2019 National Health Interview Survey questionniare redesign and weighting adjustments on early release program estimates. Centers for Disease Control and Prevention; 2020. Accessed September 2020. https://www
.cdc.gov/nchs /data/nhis/earlyrelease /EReval202009-508.pdf - 14.
- National Center for Health Statistics. National Health and Nutrition Examination Survey: NHANES Questionnaires, Datasets, and Related Documentation. Accessed 2021. https://wwwn
.cdc.gov/nchs/nhanes/ - 15.
- Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Accessed 2021. https://meps
.ahrq.gov/mepsweb/ [PubMed: 38416859] - 16.
- National Center for Health Statistics. Ambulatory Health Care Data. Updated October 23, 2023. https://www
.cdc.gov/nchs/ahcd/index.htm - 17.
- Center for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Updated August 29, 2023. https://www
.cdc.gov/brfss/ - 18.
- U.S. Centers for Medicare and Medicaid Services. Affordable Care Act. Healthcare.gov. Accessed 2022. https://www
.healthcare .gov/where-can-i-read-the-affordable-care-act/ - 19.
- Casagrande SS, McEwen LN, Herman WH. Changes in health insurance coverage under the Affordable Care Act: a national sample of U.S. adults with diabetes, 2009 and 2016. Diabetes Care. 2018;41(5):956-962. doi:10.2337/dc17-2524 [PubMed: 29475841] [CrossRef]
- 20.
- Rice T, Unruh LY, van Ginneken E, Rosenau P, Barnes AJ. Universal coverage reforms in the USA: from Obamacare through Trump. Health Policy. 2018;122(7):698-702. doi:10.1016/j.healthpol.2018.05.007 [PubMed: 29804633] [CrossRef]
- 21.
- Broaddus M, Aron-Dine A. Uninsured rate rose again in 2019, further eroding earlier progress. Center on Budget and Policy Priorities; 2020. Accessed September 15, 2020. https://www
.cbpp.org /sites/default/files /atoms/files/9-15-20health.pdf - 22.
- Bernstein H, Gonzalez D, Karpman M, Zuckerman S. Amid confusion of the public charger rule, immigrant families continue avoiding public benefits in 2019. Urban Institute; 2020. Accessed May 2020. https://www
.urban.org /sites/default/files /publication/102221 /amid-confusion-over-the-public-charge-rule-immigrant-families-continued-avoiding-public-benefits-in-2019_3.pdf - 23.
- Rogers MAM, Kim C, Lee JM, Basu T, Tipirneni R. Private insurance coverage for diabetes before and after enactment of the preexisting condition mandate of the Affordable Care Act, 2005–2016. Am J Public Health. 2019;109(4):562-564. doi:10.2105/ajph.2018.304933 [PMC free article: PMC6417562] [PubMed: 30789766] [CrossRef]
- 24.
- U.S. Centers for Medicare and Medicaid Services. Medicaid Eligibility. Accessed 2022. https://www
.medicaid .gov/medicaid/eligibility/index.html - 25.
- Lobo JM, Kim S, Kang H, et al. Trends in uninsured rates before and after Medicaid expansion in counties within and outside of the diabetes belt. Diabetes Care. 2020;43(7):1449-1455. doi:10.2337/dc19-0874 [PMC free article: PMC7305008] [PubMed: 31988065] [CrossRef]
- 26.
- Lee J, Callaghan T, Ory M, Zhao H, Bolin JN. The impact of Medicaid expansion on diabetes management. Diabetes Care. 2020;43(5):1094-1101. doi:10.2337/dc19-1173 [PMC free article: PMC7171935] [PubMed: 31649097] [CrossRef]
- 27.
- Sumarsono A, Buckley LF, Machado SR, et al. Medicaid expansion and utilization of antihyperglycemic therapies. Diabetes Care. 2020;43(11):2684-2690. doi:10.2337/dc20-0735 [PMC free article: PMC8051258] [PubMed: 32887711] [CrossRef]
- 28.
- Chen EM, Armstrong GW, Cox JT, et al. Association of the Affordable Care Act Medicaid expansion with dilated eye examinations among the United States population with diabetes. Ophthalmology. 2020;127(7):920-928. doi:10.1016/j.ophtha.2019.09.010 [PubMed: 31735405] [CrossRef]
- 29.
- Cole MB, Kim JH, Levengood TW, Trivedi AN. Association of Medicaid expansion with 5-Year changes in hypertension and diabetes outcomes at Federally Qualified Health Centers. JAMA Health Forum. 2021;2(9):e212375. doi:10.1001/jamahealthforum.2021.2375 [PMC free article: PMC8796924] [PubMed: 35977186] [CrossRef]
- 30.
- United States Diabetes Surveillance System. Diabetes Medication Use. Accessed 2022. https://gis
.cdc.gov/grasp /diabetes/diabetesatlas-surveillance.html - 31.
- Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165-2171. doi:10.2337/diacare.25.12.2165 [PMC free article: PMC1282458] [PubMed: 12453955] [CrossRef]
- 32.
- Wilson V. Diabetes education to provide the necessary self-management skills. Br J Community Nurs. 2021;26(4):199-201. doi:10.12968/bjcn.2021.26.4.199 [PubMed: 33797970] [CrossRef]
- 33.
- Carr D, Kappagoda M, Boseman L, Cloud LK, Croom B. Advancing diabetes-related equity through diabetes self-management education and training: existing coverage requirements and considerations for increased participation. J Public Health Manag Pract. 2020;26(Suppl 2):S37-S44. doi:10.1097/phh.0000000000001109 [PubMed: 32004221] [CrossRef]
- 34.
- Doucette ED, Salas J, Scherrer JF. Insurance coverage and diabetes quality indicators among patients in NHANES. Am J Manag Care. 2016;22(7):484-490. [PubMed: 27442204]
- 35.
- Amin B, Yeduri R, Tumin D, Buckman C, Bell JJ. Insurance coverage and health care use among children with diabetes. Pediatr Diabetes. 2021;22(4):605-609. doi:10.1111/pedi.13192 [PubMed: 33604962] [CrossRef]
- 36.
- Lipton BJ. Association between health insurance and health among adults with diabetes: evidence from Medicare. J Am Geriatr Soc. 2020;68(2):388-394. doi:10.1111/jgs.16238 [PubMed: 31663614] [CrossRef]
- 37.
- Benoit SR, Hora I, Pasquel FJ, Gregg EW, Albright AL, Imperatore G. Trends in emergency department visits and inpatient admissions for hyperglycemic crises in adults with diabetes in the U.S., 2006–2015. Diabetes Care. 2020;43(5):1057-1064. doi:10.2337/dc19-2449 [PMC free article: PMC7171947] [PubMed: 32161050] [CrossRef]
- 38.
- Ferdinand AO, Akinlotan MA, Callaghan T, Towne SD, Jr., Bolin J. Diabetes-related hospital mortality in the U.S.: a pooled cross-sectional study of the National Inpatient Sample. J Diabetes Complications. 2019;33(5):350-355. doi:10.1016/j.jdiacomp.2019.01.007 [PubMed: 30910276] [CrossRef]
- 39.
- Grant AK, Golden L. Technological advancements in the management of type 2 diabetes. Curr Diab Rep. 2019;19(12):163. doi:10.1007/s11892-019-1278-3 [PubMed: 31863200] [CrossRef]
- 40.
- Addala A, Auzanneau M, Miller K, et al. A decade of disparities in diabetes technology use and HbA(1c) in pediatric type 1 diabetes: a transatlantic comparison. Diabetes Care. 2021;44(1):133-140. doi:10.2337/dc20-0257 [PMC free article: PMC8162452] [PubMed: 32938745] [CrossRef]
- 41.
- Addala A, Maahs DM, Scheinker D, Chertow S, Leverenz B, Prahalad P. Uninterrupted continuous glucose monitoring access is associated with a decrease in HbA1c in youth with type 1 diabetes and public insurance. Pediatr Diabetes. Nov 2020;21(7):1301-1309. doi:10.1111/pedi.13082 [PMC free article: PMC8103618] [PubMed: 32681582] [CrossRef]
- 42.
- Everett EM, Wisk LE. Relationships between socioeconomic status, insurance coverage for diabetes technology and adverse health in patients with type 1 diabetes. J Diabetes Sci Technol. 2021;16(4):825-833. doi:10.1177/19322968211050649 [PMC free article: PMC9264432] [PubMed: 34632819] [CrossRef]
- 43.
- Jackson MA, Ahmann A, Shah VN. Type 2 diabetes and the use of real-time continuous glucose monitoring. Diabetes Technol Ther. 2021;23(Suppl 1)(S1):S27-S34. doi:10.1089/dia.2021.000710.1089/dia.2021.0007 [PMC free article: PMC7957379] [PubMed: 33534631] [CrossRef] [CrossRef]
- 44.
- Janapala RN, Jayaraj JS, Fathima N, et al. Continuous glucose monitoring versus self-monitoring of blood glucose in type 2 diabetes mellitus: a systematic review with meta-analysis. Cureus. 2019;11(9):e5634. doi:10.7759/cureus.5634 [PMC free article: PMC6822918] [PubMed: 31700737] [CrossRef]
- 45.
- Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-374. doi:10.7326/m16-2855 [PubMed: 28828487] [CrossRef]
- 46.
- Bergenstal RM, Kerr MSD, Roberts GJ, Souto D, Nabutovsky Y, Hirsch IB. Flash CGM is associated with reduced diabetes events and hospitalizations in insulin treated type 2 diabetes. J Endocr Soc. 2021;5(4):bvab013. doi:10.1210/jendso/bvab013 [PMC free article: PMC7901259] [PubMed: 33644623] [CrossRef]
- 47.
- Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G. Use of flash glucose-sensing technology for 12 months as a replacement for blood glucose monitoring in insulin-treated type 2 diabetes. Diabetes Ther. 2017;8(3):573-586. doi:10.1007/s13300-017-0255-6 [PMC free article: PMC5446381] [PubMed: 28401454] [CrossRef]
- 48.
- Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C, Group DS. Continuous glucose monitoring in older adults with type 1 and type 2 diabetes using multiple daily injections of insulin: results from the DIAMOND trial. J Diabetes Sci Technol. 2017;11(6):1138-1146. doi:10.1177/1932296817704445 [PMC free article: PMC5951040] [PubMed: 28449590] [CrossRef]
- 49.
- Wang Y, Park J, Li R, Luman E, Zhang P. National trends in out-of-pocket costs among U.S. adults with diabetes aged 18–64 years: 2001–2017. Diabetes Care. 2021;44(11):2510-2517. doi:10.2337/dc20-2833 [PMC free article: PMC9578147] [PubMed: 34429323] [CrossRef]
- 50.
- Park J, Zhang P, Wang Y, Zhou X, Look KA, Bigman ET. High out-of-pocket health care cost burden among Medicare beneficiaries with diabetes, 1999–2017. Diabetes Care. 2021;44(8):1797-1804. doi:10.2337/dc20-2708 [PMC free article: PMC8376067] [PubMed: 34183427] [CrossRef]
- 51.
- Neilson LM, Munshi KD, Peasah SK, et al. Changes in type 2 diabetes medication utilization and costs in the United States, 2014–2019. Med Care. 2021;59(9):789-794. doi:10.1097/mlr.0000000000001597 [PubMed: 34183622] [CrossRef]
- 52.
- Zhou X, Shrestha SS, Shao H, Zhang P. Factors contributing to the rising national cost of glucose-lowering medicines for diabetes during 2005–2007 and 2015–2017. Diabetes Care. 2020;43(10):2396-2402. doi:10.2337/dc19-2273 [PMC free article: PMC7510041] [PubMed: 32737138] [CrossRef]
- 53.
- Laxy M, Zhang P, Benoit SR, et al. Trends in total and out-of-pocket payments for insulin among privately insured U.S. adults with diabetes from 2005 to 2018. Diabetes Care. 2021;44(10):e180-e182. doi:10.2337/dc20-2529 [PubMed: 34348995] [CrossRef]
- 54.
- Shao H, Laxy M, Benoit SR, Cheng YJ, Gregg EW, Zhang P. Trends in total and out-of-pocket payments for noninsulin glucose-lowering drugs among U.S. adults with large-employer private health insurance from 2005 to 2018. Diabetes Care. 2021;44(4):925-934. doi:10.2337/dc20-2871 [PubMed: 33563653] [CrossRef]
Appendices
APPENDIX A1.
Types of Health Insurance Coverage Among Adults, by Diabetes Status, Age, and Race/Ethnicity, U.S., 2019
APPENDIX A2.
Trends in Medicare Advantage Among Adults Age ≥65 Years With Diabetes, by Demographic Characteristics, U.S., 2010–2019
APPENDIX A3.
Trends in Medicare Advantage Among Adults Age ≥65 Years Without Diabetes, by Demographic Characteristics, U.S., 2010–2019
APPENDIX A4.
Prevalence of Health Insurance Coverage Among Adults Age 18–64 Years, by Diabetes Status and Demographic Characteristics, U.S., 2009, 2019, and 2021
APPENDIX A5.
Prevalence of Quality of Care and Health Care Utilization Among Adults Age 20–64 Years With Diabetes, by Health Insurance Status and Race/Ethnicity, U.S., 2017–March 2020
Drs. Casagrande, Park, Herman, and Bullard reported no conflicts of interest.
Publication Details
Author Information and Affiliations
Authors
Sarah S. Casagrande, PhD, 1 Joohyun Park, PhD,2 William H. Herman, MD, MPH,3 and Kai McKeever Bullard, PhD, MPH2.
1 Joohyun Park, PhD,2 William H. Herman, MD, MPH,3 and Kai McKeever Bullard, PhD, MPH2.Affiliations
Division of Epidemiology and Biostatistics
Silver Spring, MD
Division of Diabetes Translation
Atlanta, GA
School of Medicine
Department of Internal Medicine
Division of Metabolism, Endocrinology, and Diabetes
School of Public Health
Department of Epidemiology
Ann Arbor, MI
 Corresponding author.
Corresponding author.Publication History
Initial Posting: December 20, 2023.
Copyright
Diabetes in America is in the public domain of the United States. You may use the work without restriction in the United States.
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Bethesda (MD)
NLM Citation
Casagrande SS, Park J, Herman WH, et al. Health Insurance and Diabetes. 2023 Dec 20. In: Lawrence JM, Casagrande SS, Herman WH, et al., editors. Diabetes in America [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); 2023-.