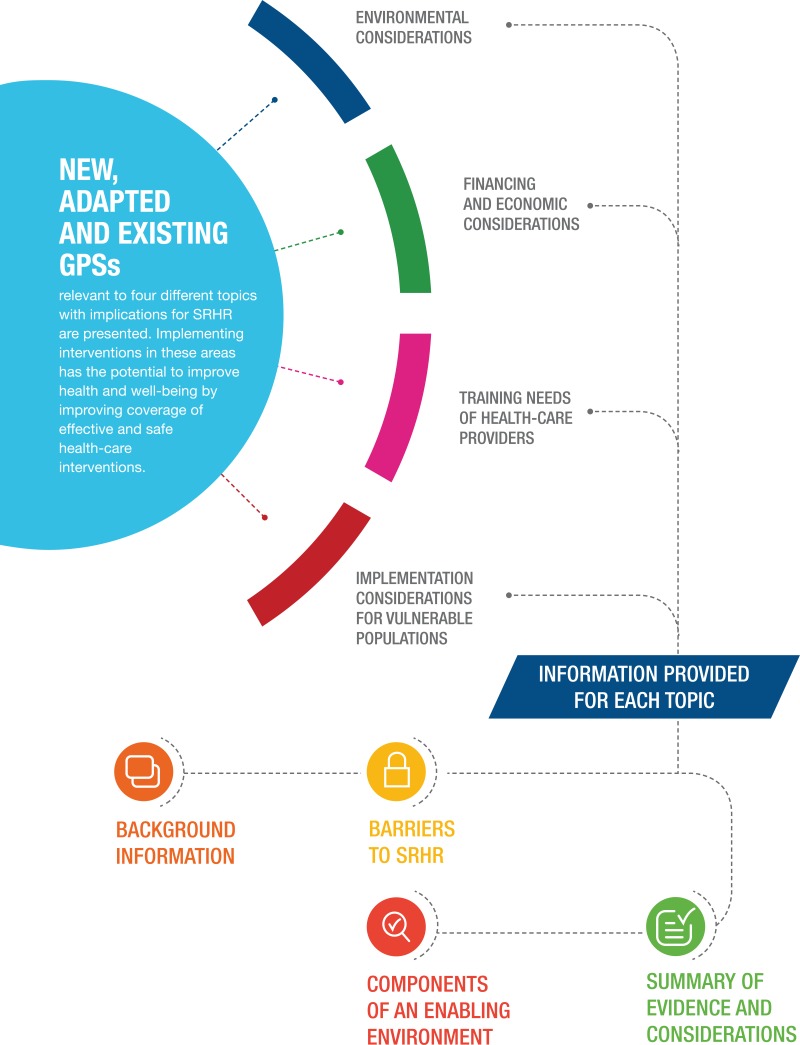
5.5.1. New good practice statements on self-care for people of all ages, those in humanitarian settings, and by use of digital health interventions
New good practice statement on the life-course approach to SRHR
- GPS 6 (NEW)
Sensitization about self-care interventions, including for SRHR, should be tailored to people’s specific needs across the life course, and across different settings and circumstances, and should recognize their right to sexual and reproductive health across the life course.
i. Background
Under a life-course approach, health and the risk of disease are understood as the result of the life experiences, social and physical exposures throughout an individual’s life, from gestation to late adulthood (35). This approach promotes timely interventions to support the health of individuals at key life stages, calling for actions targeting whole societies as well as the causes of disease and ill health, rather than just targeting the consequences in individuals. In sum, a life-course approach to health and well-being means recognizing the critical, interdependent roles of individual, inter-generational, social, environmental and temporal factors in the health and well-being of individuals and communities (36).
The main outcome of the life-course approach is functional ability, which is determined by the individual’s intrinsic capacity in their interactions with their physical and social environments and which is, thus, interdependent with the realization of human rights (37). Functional ability allows people to do what they value doing, which enables well-being at all ages, from gestation and birth, through infancy, early childhood, adolescence and adulthood, to older adulthood (38).
ii. Barriers to SRHR
A lack of systematic knowledge about the way health at different life stages interrelates and accumulates through a lifetime and generations is one of the main barriers to the implementation of the life-course approach to support health and well-being, including SRHR. There are few studies on this issue, most of them focusing on populations in the Global North. An obstacle to improving the understanding of health through time is the current focus on single diseases and specific age groups.
Age-based discrimination is another of the main barriers standing in the way of a better understanding of the SRHR needs of populations in particular age stages; for instance, notions about the sexual lives, needs and health of older populations and adolescents are often clouded by stereotypes. Discrimination against older populations has received increased attention since the 1980s, when the term “ageism” was coined to refer to this particular kind of age-based discrimination (39).
Better understanding of these barriers – and of why people will access self-care rather than facility-based health services – can allow for better use and uptake of self-care interventions. Reducing age-based discrimination and shifting the focus of research and action so that they take into account temporality and interconnectedness is critical to better tailor policy and actions.
iii. Components of an enabling environment that will address the barriers and support SRHR
Age-friendly environments will enable the SRHR needs of populations to be better addressed across the entire age spectrum. Fostering age-friendly environments, which entails reducing ageism, is part of WHO’s Global Strategy on Ageing and Health (40). The United Nations and the Decade of Action on Healthy Ageing, to be launched in 2020 (41) recognize healthy ageing as a contributing factor to the attainment of the Sustainable Development Goals (SDGs) (42).
Based on case studies carried out by WHO on the implementation of the life-course approach to health in the small European countries of Iceland and Malta, three additional enabling factors were identified. The first entails strengthening collaboration across different government areas, sectors and society, as it was observed that planning and action benefitted from the perspectives and involvement of all actors involved. The second is about making health-care interventions sensitive and responsive to equity and gender, as these two factors are often at the root of disadvantages lasting an individual lifetime and persisting through generations. Finally, the third identified enabling factor was allocating time and resources to monitoring and knowledge exchange; these two activities are key to ensure the adoption and ongoing improvement and durability of the life-course approach and actions (43).
iv. Summary of the evidence and considerations of the GDG
The case of older populations illustrates well the potential benefits of the adoption of a life-course approach to health, particularly SRHR. “Older adults” remains too broad a category, as it is often shorthand for all adults in the second half of life (44). However, older adulthood comprises different stages of life that should be differentiated and better understood in order to meet the SRHR needs of specific stages. WHO currently identifies three age categories in older adulthood: middle adulthood (age 50–64 years) and two age groups in later adulthood (ages 65–79 and 80+) (45). Sexual health remains a key consideration among older adults (46). According to the few systematic reviews on the sexual health of older adults, there is also a lack of diversity in research, as most systematic studies on the matter are based on populations of older adults living in the Global North (47).
A life-course approach that is sensitive, respectful and knowledgeable about the particular challenges and opportunities at all ages would also help reduce age-based discrimination. Stereotypes regarding the sexualities and sexual lives of older adults persist despite various studies that have shown that sex and pleasure are integral to the lives and well-being of older adults. Although this issue remains understudied, the available evidence suggests that supporting older adults’ intrinsic capacities for healthy living includes supporting them in their choice to enjoy safe and fulfilling sexual relationships and sexual pleasure as they age. In order to support informed choices, improving health literacy of older adults regarding accurate information, services and self-care for SRHR remains of the utmost importance.
New good practice statement on the use of digital health interventions to support the use of self-care interventions
- GPS 7 (NEW)
Digital health interventions offer opportunities to promote, offer information about and provide discussion forums for self-care interventions, including for SRHR.
i. Background
The provision of accurate and tailored information about specific health-care interventions and technologies, including through mobile devices, is important to promote safe and effective SRHR-related self-care. To this end information is needed to:
facilitate access (e.g. with details of potential sources/access points);
promote appropriate use of an intervention/technology, through comprehensible (step-by-step) instructions;
inform potential users about likely physical and emotional ramifications, plus potential side-effects and contraindications; and
advise potential users about the circumstances under which they should seek care and how to do so.
ii. Barriers to SRHR
Self-care for SRHR has perhaps the greatest potential to address unmet needs or demands in marginalized populations or in contexts of limited access to health care, including, for instance, self-managed medical abortion in countries where abortion is illegal or restricted. In such contexts, a lack of access to specific interventions is often accompanied by a lack of appropriate information regarding the intervention (48) (e.g. when young people obtain emergency contraception from pharmacists but immediately discard the packaging and information sheet because of its potential to incriminate them) and reticence to discuss the intervention because of the associated stigma (49).
Many of the studies of digital health interventions, including use of eHealth and “mobile health” (mHealth, a component of eHealth), which often facilitate targeted client communication or provider-client telemedicine, recognize issues around access (particularly in relation to the availability of mobile phones and connectivity) as well as potential issues of confidentiality. There are also limitations in terms of the research conducted on these interventions; data on health outcomes are limited and the studies rarely use a rigorous research design (50).
iii. Components of an enabling environment that will address the barriers and support SRHR
Digital health technologies offer potential conduits for information beyond more traditional information sources in the formal health system. Digital health technologies encompass a variety of approaches to information provision, including targeted provider-to-client communications; client-to-client communications; and on-demand information services for clients (51). In terms of on-demand SRHR information, the Internet is popular, particularly because the information online is available, affordable, anonymous and accessed in private (52, 53). Online discussion forums – using social media or a range of applications (apps) – can be sources of peer-to-peer information around SRHR self-care technologies. With regard to information provision via mobile phones (text message/SMS or apps on smart phones), recent reviews have demonstrated high feasibility and acceptability of the provision of SRHR-related information, with studies also demonstrating knowledge and behaviour change (54).
iv. Summary of the evidence and considerations of the GDG
A recent systematic review of studies of adolescents accessing SRHR information online highlighted a demand for information and education about sexual experiences (not just technical information) and reviewed the impact of accessing information in this way in terms of behaviour change. The review also highlighted how demand for information varied across the adolescent age groups and showed that adolescents were generally good at evaluating information. However, there is a lack of research on the role of social media in providing SRHR-related information. The relatively few studies undertaken highlight issues with measuring impact, limitations of study designs and a lack of standard reporting (55).
Recent reviews highlight how the effectiveness of digital health interventions to provide appropriate information for safe and effective self-care for SRHR is predicated on consideration for: (i) potential users’ access to technology/digital devices, including limited connectivity; (ii) diversity and changes in the types of delivery channels (e.g. text, voice, apps, etc); (iii) age- and population-specific (e.g. gender, sexuality, disability) information priorities and needs; (iv) the need to tailor content and maintain fidelity of messages; (v) concerns about confidentiality; and (vi) current levels of literacy, as well as digital and health literacy.
Additionally, the WHO guideline: recommendations on digital health interventions for health system strengthening presents 10 recommendations on digital health interventions, based on an assessment of their effectiveness (benefits and harms), as well as considerations of resource use, feasibility, equity and acceptability (values and preference) (56).
New good practice statement on support for self-care interventions in humanitarian settings
- GPS 8 (NEW)
Provision of tailored and timely support for self-care interventions, including for SRHR, in humanitarian settings should be in accordance with international guidance, form part of emergency preparedness plans and be provided as part of ongoing responses.
i. Background
In 2015, UNHCR – the United Nations Refugee Agency – estimated that the global population of forcibly displaced people exceeded 65 million for the first time in history. Of those needing humanitarian assistance, it is estimated that approximately 1 in 4 are women and girls of reproductive age. The diversity in populations (refugees, asylum seekers, internally displaced persons), settings (from refugee camps to urban areas), circumstances (conflict, post-conflict, natural disasters) and their varying access to rights (e.g. citizens versus non-citizens) all add to the complexity of providing quality care in challenging circumstances (57). With approximately 40% of refugees experiencing displacement for over five years, and many for over 20 years, this underscores the need for a life-course approach to health care for refugees (58).
ii. Barriers to SRHR
The ability to realize SRHR in the context of humanitarian crises is constrained by a complex interplay of factors, including increased poverty; gender-based violence; trauma and mental health challenges; limited access to and quality of health care; breakdown of familial, social and community networks; and problematic living conditions (59). Language also often presents a barrier to health-care access and may result in avoidance of care, misdiagnosis and decreased medical compliance. Thus, there is a need to adapt innovative SRHR service-delivery models for humanitarian contexts (60).
iii. Components of an enabling environment that will address the barriers and support SRHR
Health system strengthening during emergencies remains essential to support and facilitate access to self-care interventions for SRHR. Communities also respond on their own to crises, developing informal yet strong social support systems and an enabling environment. All these are entry points to supporting individuals to improve health outcomes (57). The growing evidence base on implementing comprehensive approaches to delivery of the Minimum Initial Service Package (MISP) will support improved health outcomes, but there is still much work to be done in this field (61).
iv. Summary of the evidence and considerations of the GDG
Given the lack of longitudinal data or studies with an adequate control comparison group, innovative ways of collecting data should be tested, such as using information and communications technologies (ICTs) that are widely used by many conflict-affected populations (e.g. WhatsApp). These data-collection methods may prove beneficial for researchers, health-care providers and organizations seeking to collect health outcome data at the individual-level, including from populations on the move who have traditionally been challenging to follow up (60). There is also a need for innovation in establishing stronger referral and follow-up systems in humanitarian settings to ensure that health outcome indicators used to assess effectiveness are truly the most appropriate for this purpose. Researchers should also consider use of alternative study designs where standard randomized controlled trials are not operationally or ethically possible (60).