Abstract
BACKGROUND
Children with ataxic cerebral palsy have unsteady movements and poor balance. Many therapeutic interventions are used to improve their upper and lower functioning.
AIM
To assess the effectiveness of virtual reality (VR) on balance impairment in ataxic cerebral palsy children.
DESIGN
RCT.
POPULATION
Sixty-four children with ataxic cerebral palsy.
METHODS
Children were randomly assigned into two equal groups with 32 patients in each group. The control group received a specially developed physical therapy program and the VR group received VR training on a Wii balance board in addition to the control group’s program. For three successive months the intervention program was implemented three times a week for both groups. Stability indices (overall, anteroposterior, and mediolateral) were measured using the Biodex balance system and Pediatric Balance Scale (PBS) at baseline and after three months of intervention for both groups.
RESULTS
At the beginning of the intervention, there were no statistically significant differences between the two groups (P>0.05). However, following three months of the intervention, there was a statistically significant decline in the stability index scores., as well as a statistically significant improvement in the score of the PBS in both groups with a notable advancement in favor of the VR group (P≤0.05).
CONCLUSIONS
Adding VR training on a Wii balance board to a designed physical therapy program has a significant impact on improving balance deficits in ataxic cerebral palsy children.
CLINICAL REHABILITATION IMPACT
VR has a therapeutic effect on improving balance that may result in better and more efficient rehabilitation program of children with ataxic cerebral palsy.
Key words: Cerebral palsy, ataxic; Virtual reality; Balance
Cerebral palsy is the most common disorder affecting motor function in childhood.1, 2 It is clinically classified according to the primary kind of motor involvement into spastic, dyskinetic, dystonic, and ataxic subgroups. Ataxic cerebral palsy represents 5-10% of all cases. It is caused by cerebellar damage and is characterized by proximal instability, involuntary tremors, clumsiness, loss of coordination, and poor balance.3
Children with ataxic cerebral palsy have a loss of muscular control in their arms and legs, leading to unsteady movements, poor balance, and incoordination which limit everyday activities and increase the risk of falling. They walk with large sways of the center of pressure, mainly in an anteroposterior direction with irregular uncoordinated stepping.4
Conventional physical therapy modalities for balance disorder in ataxic cerebral palsy include balance training using weights, foot sensory stimulation, core stability, and home-based exercises.5 Virtual reality (VR) gaming is a modern technology which provides a variety of unique interventions that need patients’ full attention and active participation.6 It facilitates the interaction in multisensory tasks that are mainly used in activities of daily living such as hand skills, manipulation, mobility, balance, and cognition.1
The Wii balance board is a popular VR design used to promote balance and fitness while entertaining users. It provides children with challenges, increases curiosity, and promotes fantasy for them to fully engage with the intervention.7
VR is more motivating than traditional exercises for children as it provides motivation, quantitative recording of the balance changes, and visual feedback.8 Several studies demonstrated the efficacy of the Wii balance board for improving balance in spastic and dyskinetic cerebral palsy, down syndrome, and acquired brain injury.9-11 Also, other studies reported its effect in improving cognitive function in traumatic brain injury and enhancing gait and balance after stroke and SCI.12 However, till now studies on ataxic cerebral palsy were case reports and no randomized controlled trial was performed. So, our study aimed to assess the efficacy of VR training on a Wii balance board in addition to a physical therapy rehabilitation program on balance impairment in ataxic cerebral palsy children. We hypothesized that adding VR training on a Wii balance board to the physical therapy rehabilitation program would have a favorable impact on balance impairment in ataxic cerebral palsy children after three months of training.
Materials and methods
A single-blinded (children) randomized controlled experiment was carried out in the Cairo University faculty of physical therapy outpatient clinic between November 2022 to April 2024.
Blinding and allocation
This study was authorized by Cairo University’s Faculty of Physical Therapy Ethical Committee for Clinical Research (P.T.REC/012/004402), and it was also registered on ClinicalTrials.gov. and has the NCT05411328 identification number. Before starting the study procedures, each child’s parents signed an informed consent form to ensure their satisfaction and informed them that they have the right to withdraw from the study without any penalty by keeping their data confidential.
Seventy ataxic cerebral palsy children were initially assessed for eligibility. Five children failed to convene the inclusion criteria, one refused to enroll. The remaining sixty-four children were assigned randomly into two groups of equal numbers (control and VR) by a blinded independent researcher; selection bias was minimized by using random allocation software.13 Figure 1 shows the flow chart of children and randomization of the study.
Figure 1.
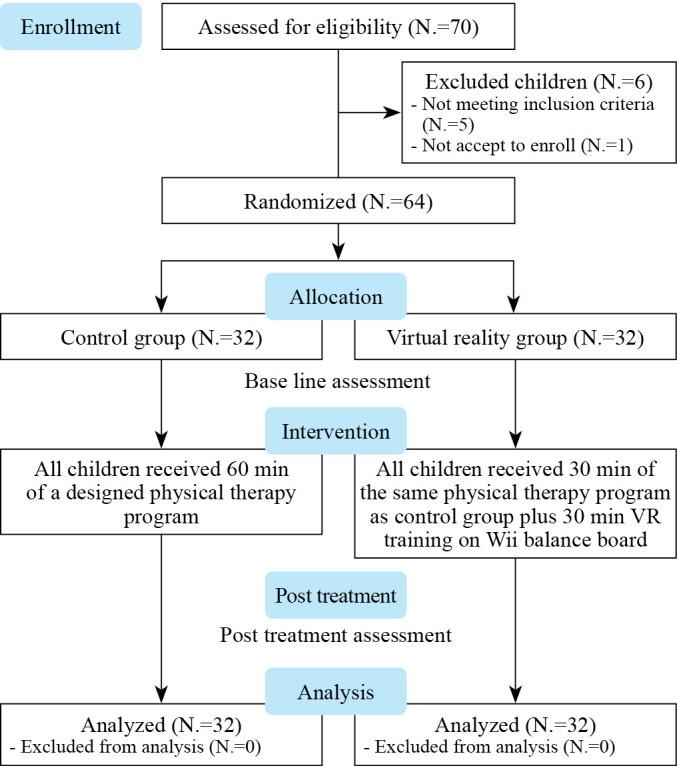
—Flow chart of children randomization.
Sixty-four children with ataxic cerebral palsy were enrolled in our study. They were referred and diagnosed by a pediatric neurologist and diagnosis was confirmed by history of brain damage in addition to MRI finding that revealed atrophy of cerebellum. Their ages ranged from nine to fourteen years. All children had incoordination, tremors, balance disturbance and were able to walk independently without assistance with ataxic gait. The severity level of motor impairment was level I and II according to GMFCS.14 All children had sufficient intelligence to follow the instructions during testing and training procedures (IQ scores >70 according to Stanford-Binet Intelligence Test).15 We exclude children who scored ≥28 according to the pediatric symptom checklist that had a degree of behavioral and emotional dysregulation2 and children with structural abnormalities, visual or auditory impairments, or a history of epilepsy.
Children in the control group underwent sixty minutes of a specially developed physical therapy program. While children in the VR group underwent the same specially developed physical therapy program as control group for 30 min adding VR training on the Wii balance board for thirty min. with a total session duration of sixty min.16
The specially developed physical therapy program included stretching hamstrings, and calf muscles, rhythmic stabilization for shoulder and pelvic girdle, balance training (from different positions such as kneeling, half kneeling, and standing), standing on a balance board; standing on the single leg; stoop and recovery; gait training on a balance beam and stepper; walking on wedges and stair climbing.17-20
VR training was performed by using Nintendo Wii Fit Plus with balance board,16 a device attached to a sufficiently distant screen at which the center of pressure’s displacement on the device balance board was displayed. The device provides a wide variety of games, in our study, tennis,20 baseball,21 and bowling games22 were selected. Tennis and baseball games were used to increase the strength of muscles in both upper and lower limbs (e.g. rectus femoris, biceps femoris, vastus medialis, gastrocnemius, and gluteus maximus muscles),20, 21 while bowling games were used to enhance balance and core muscles strength.22
During the intervention process, the child stood on the balance board and used visual feedback to control the shifting of the screen’s center of pressure. The child can change the center of gravity in several planes (dynamic balance) and keep the center of gravity at a constant location (static balance). The therapist also gave verbal feedback for each game according to the balance abilities of each child. All games were played at the basic level.
An illustrative training trial of VR games was performed before starting the treatment sessions. Each child was asked to complete one round of each game. The training trial included multiple verbal instructions and explanations on movements used during playing the intervention games like lateral weight shifting, stepping side/forward/backward, and squatting while controlling the movements of the upper extremities. The physiotherapist stood next to each child asking him to collect as many points as possible and keeping him from falling over while playing the activities due to an extreme body movement. Both groups received the treatment regimen three times a week for three consecutive months conducted by a certain therapist and to avoid bias; examination was done by another therapist.
In the tennis game
The child was asked to hold the Wii remote as if it was the grip of a tennis racket and swing it. The racquet was timed to strike the ball so that it bounced to the left (forehand early strike) or right (forehand late strike). The child was asked to hit a forehand shot, when he early hit the ball, it hooked and aimed to the player’s left. When he later hit the ball (it closed his body), it sliced and aimed to the right.
In Baseball game
Baseball games on the Wii are not played in the same way as traditional baseball. There is only batting and pitching involved. For batting: the child was asked to hold the remote with both hands; on the screen, the child showed his model, and the pitcher threw the ball. The child observes the bat’s movement in relation to the ball’s position as they are swinging. This helps the child learn about the swing’s direction and speed. Furthermore, a sound indicating the swing’s speed is produced during the swing. The child hears a crack and hears applause from the crowd when the bat makes contact with the ball. The remote is also vibrating simultaneously. The child observes the ball’s trajectory after the bat strikes it. The child can tell if the batter struck the ball too early or too late by hearing the audience’s displeasure if the batter misses the ball. The announcer reports the result of the batting bat after every swing. For pitching: the child can release the ball for the pitch by moving their arm in a variety of ways while holding the remote in one hand. The child hears and sees the ball land in the catcher’s mitt. The key to an effective pitch is to accelerate the child’s swing movement.23
In the bowling game
The child attempted to knock down 10 pins with a ball, the child was asked to hold the B button to throw and was asked to release it when he was ready to throw. The spin was quite amazing, and it followed a very realistic curve that led to the ball’s path. The path taken and, consequently, the number of pins dropped are determined by the degree of twist applied at release as well as the moment of the ball’s release. It is therefore best to bowl normally and fully for success. At all games, the child played against the computer.
All children were examined by Biodex Balance System (BBS) for measuring stability indices and the Pediatric Balance Scale (PBS) at baseline and after three months of intervention for both groups.
Stability indices were assessed by using the BBS (Model 945-302, software version 3.12, New York). It is an objective method used to evaluate and train subjects with balance problems.24 The system is comprised of a circular platform with supports. It is capable of a 20° tilt from the horizontal in different directions. The actuator of the system, which is based on a microprocessor, regulates how much the platform’s surface is unstable. Changing the surface instability from a minimally unstable level (8) (minimally unstable) to very unstable level (1) is possible. According to our previous pilot research, Level 8 was utilized to evaluate balance in all children. Each child was instructed to keep his center of mass in the center of a concentric circle that was displayed on the screen in front of them to measure his balance indices. The device determines the variation from the center, which is reported as a balancing index, and records the actual postural sway. A larger variation that is measured as a higher balance index score reflects more postural sway. The test was composed of three trials, each lasting 20 seconds and interspersed with a 25-second rest. The three trials’ average value was calculated. The system measures the overall stability index (OASI), anteroposterior stability index (APSI), and mediolateral stability index (MLSI) that calculate a child’s ability to keep his balance in all directions, forward-backward directions, and medial-lateral directions respectively.25-28
The PBS is a modified version of the Berg Balance Scale intended to assess children’s functional balance abilities. It is a valid and reliable tool.29 The intra-rater reliability and interrater reliability were (ICC=0.998, ICC=0.997 respectively), it consists of 14 tasks; simple mobility tasks (e.g., transfers, standing unsupported, sit-to-stand) and more difficult tasks (e.g., tandem standing, turning 360°, single-leg stance). Every item has a grade of 0 to 4, and the total score has a grade of 0 to 56. The maximum score is 56 indicates better balance and reflects the child’s ability to maintain a static position, alter positions, and reduce the basis of support for each task from different positions. Three trials are allowed, and the best performance was measured for analysis.29
The sample size was calculated by using G power program version 3.1, Heinrich-Heine-University, Düsseldorf, Germany based on F tests (MANOVA: Special effects and interactions), Type I error (α)=0.05, power (1-α error probability)=0.80, Pillai V=0.20 and effect size f2 (V)=0.1111. Twenty-two children were the ideal bare minimum sample size for this investigation. According to pilot research with ten participants, the effect size was computed considering the outcome measures. As a result, the projected sample size for all patients was twenty-two, and when dropouts were taken into account from the time of randomization to the conclusion of the treatment regimen, the number of children climbed to 32.
Statistical analysis
An unpaired t-test was used to compare the subject characteristics of the groups. The data was tested for normal distribution using the Shapiro-Wilk Test. To evaluate the homogeneity between groups, Levene’s Test for homogeneity of variances was used. A mixed MANOVA was used to investigate how the therapy affected the PBS, OASI, APSI, and MLSI. The Bonferroni adjustment was used in post-hoc tests to perform multiple comparisons later. All statistical tests were conducted with a significance level of P<0.05. The statistical package for social studies (SPSS) version 25 for Windows was used for all statistical analysis (IBM SPSS, Chicago, IL, USA).
Results
Subject characteristics
Table I shows the subject characteristics of VR and control groups. There was no significant difference between groups in age, weight, height and BMI (P>0.05).
Table I. —Comparison of subject characteristics between VR and control groups.
| VR group Mean±SD |
Control group Mean±SD |
MD | t-value | P value | |
|---|---|---|---|---|---|
| Age (years) | 10.72±1.25 | 11.16±1.39 | -0.44 | -1.32 | 0.19 |
| Weight (kg) | 44.03±6.15 | 43.47±9.27 | 0.56 | 0.29 | 0.77 |
| Height (cm) | 140.72±8.98 | 138.47±8.42 | 2.25 | 1.03 | 0.31 |
| BMI (kg/m2) | 22.35±3.21 | 22.85±5.30 | -0.5 | -0.46 | 0.65 |
SD: standard deviation; MD: mean difference; P value: probability value.
Effect of treatment on PBS, OASI, APSI and MLSI
Mixed MANOVA revealed a significant interaction effect of treatment and time (F=19.70, P=0.001, Partial eta squared=0.57). There was a significant main effect of treatment (F=9.16, P=0.001, Partial eta squared=0.38). There was a significant main effect time (F=454.50, P=0.001, Partial eta squared=0.96).
Within group comparison
There was a significant increase in PBS and a significant decrease in OASI, APSI, and MLSI in both groups post-treatment compared with pre-treatment (P>0.001). The percentage of improvement in PBS, OASI, APSI, and MLSI of the VR group was 85.23, 20.27, 33.40 and 33.91% respectively, and that in the control group was 51.51, 13.50, 26.71 and 22.42% respectively (Table II).
Table II. —Mean PBS, OASI, APSI, and MLSI pre and post-treatment of VR and control groups.
| Pre-treatment Mean±SD |
Post treatment Mean±SD |
MD (95% CI) | % of change | P value | |
|---|---|---|---|---|---|
| PBS | |||||
| VR group | 22.34±3.21 | 41.38±2.72 | -19.04 (-20.51, -17.56) | 85.23 | 0.001 |
| Control group | 23.78±3.89 | 36.03±2.85 | -12.25 (-13.72, -10.78) | 51.51 | 0.001 |
| MD (95% CI) | -1.44 (-3.22, 0.34) | 5.35 (3.95, 6.73) | |||
| P=0.11 | P=0.001 | ||||
| OASI | |||||
| VR group | 5.40±0.56 | 3.32±0.77 | 2.08 (1.83, 2.32) | 20.27 | 0.001 |
| Control group | 5.55±0.47 | 4.36±0.64 | 1.19 (0.95, 1.43) | 13.50 | 0.001 |
| MD (95% CI) | -0.15 (-0.41, 0.10) | -1.04 (-1.39, -0.68) | |||
| P=0.23 | P=0.001 | ||||
| APSI | |||||
| VR group | 5.21±0.55 | 3.47±0.36 | 1.74 (1.52, 1.94) | 33.40 | 0.001 |
| Control group | 5.13±0.58 | 3.76±0.38 | 1.37 (1.16, 1.59) | 26.71 | 0.001 |
| MD (95% CI) | 0.08 (-0.21, 0.36) | -0.29 (-0.47, -0.10) | |||
| P=0.59 | P=0.003 | ||||
| MLSI | |||||
| VR group | 4.60±0.35 | 3.04±0.42 | 1.56 (1.38, 1.74) | 33.91 | 0.001 |
| Control group | 4.55±0.46 | 3.53±0.38 | 1.02 (0.84, 1.20) | 22.42 | 0.001 |
| MD (95% CI) | 0.05 (-0.15, 0.26) | -0.49 (-0.69, -0.29) | |||
| P=0.60 | P=0.001 |
SD: standard deviation; MD: mean difference; CI: confidence interval; P value: probability value.
Between-group comparison
There was a significant increase in PBS and a significant decrease in OASI, APSI, and MLSI of the VR group compared with that of the control group post-treatment (P<0.01) (Table II).
Discussion
Ataxic cerebral palsy children struggle to regulate their movements. They have trouble with accurate motions and are unsteady as well as static and dynamic balance. These problems increase the chance of falling and impede daily living activities independence. So, our trial aimed to evaluate the efficacy of VR using Wii balance board training on balance impairment in ataxic cerebral palsy children. The findings showed that there was a statistically significant decline in stability indices measured by BBS including OASI, APSI, MLSI and a significant increase in PBS post-treatment in both groups with more improvement in favor of VR group.
Our participant’s age was limited to 9-14 years old as postural stability and adjustments were associated with age. The capability to control anterior-posterior adjustments became increasingly apparent, and sensory development began with the visual system, then the proprioceptive system, and ultimately the vestibular system, achieving functional maturity at nine years of age. Children of seven years seem to have a distinct singularity in their postural control.30 Additionally, children with cerebral palsy always lose their balance between the ages of four and fourteen years.31
The result of this study revealed a statistically significant decrease in Biodex stability indices as well as a statistically significant improvement in PBS scores in both groups. The reduction of balance indices indicates proper neuromuscular control as they exhibit the complete proprioceptive reflex control necessary to generate timely coordinated movements that are required to maintain balance and equilibrium.32 This may be attributed to the restorative goal of physical therapy exercises for ataxic children that focus on improving the strength and endurance of the trunk-stabilizing muscles, as well as the link between brain control and the musculoskeletal system.25 Exercises also increase proprioceptive stimulation33 and encourage better organization and integration of sensory information at various levels of the central nervous system.34 They increase the nervous system’s capability to anticipate the loss of balance as adequate sensorimotor processing enables adaptability to external disturbances and the enhancement of appropriate neuromuscular response and potential motor adjustment mechanism optimization by correcting programming errors in movement direction, force, and execution.35 Exercises also induce motor learning as they shift the learning process from the implicit sequence of learning to the explicit sequence of learning.36
This is supported by Keller and Bastain,37 who concluded that a six-week home-based balance training regime improved the clinical and laboratory measures of mobility in patients with cerebellar ataxia. Also, Mulligan et al.38 reported that 30 min of the physical therapy program, 3/week for eleven weeks provided improvement of postural control in a non-progressive ataxic child.
The advanced improvement in the VR group may be due to the accumulating effect of VR and therapeutic exercise. VR training can aid motor rehabilitation through different mechanisms, including augmented sensory feedback, reduced cognitive load,39 reduced musculoskeletal co-activation, and increased arousal and motivation.40
VR provides multisensory environments that include visual feedback, repetitive movements requiring constant weight shifting between the feet and from heel to toes, mechanical stimulation of proprioceptors at this level, enhanced perception for complex tasks, and kinesthetic movements that activate proprioceptors in the trunk, upper limbs, and lower limbs.41 To conduct the appropriate postural adjustment for each patient, this information ascends to the central nervous system and descends through the spinal cord.42
This is consistent with Pourazar et al.,43 who reported that VR training can successfully improve the balance ability in cerebral palsy children. Also, Winfried et al.,44 concluded that VR training in the form of x-box had a great impact on improving balance capacities characteristics of gait for 10 progressive spinocerebellar ataxic children after 8 weeks of coordinative training.
Our results are also supported by Shakiba et al.,3 who reported that 20 minutes of Wii Balance Board training for twelve weeks has a great effect on improving the functional balance of ataxic CP children. Also, Silva et al.45 concluded that 30 minutes of Wii Fit Plus game, 3/a week for four months in addition to floor kinesiotherapy treatment once a week improves the static and dynamic balance in an ataxic cerebral palsy child. Schiavinato et al.,46 reported that 10 rehabilitation sessions with Wii Fit Plus videogame had a great impact on improving balance in patients with cerebellar dysfunction.
Also, Staiano et al.,47 reported that active video games like Wii fit increase fine and gross motor function and enhanced their daily activity on cerebral palsy children and concluded that Wii fit can be utilized as a home-based or a school-based solution for rehabilitation.
Wang and Reid48 found improvement in lower limb function, weight distribution on anterior-posterior, medial-lateral axes, and loading on the lower limb, in addition to an increase in the distance of walking using forearm crutches with a decrease of center of pressure sway and reliance on a walker in cerebral palsy children after 4 weeks of Wii system intervention. Some limitations of our study should be considered. First, the findings of this study should be investigated with a longer duration of treatment and to provide for follow-up period to ensure the maintenance of our statistical findings over time. Second, the psychosocial aspects of a child’s improvement have not been investigated, which could have an impact on the outcome measures.
Conclusions
The findings of our study showed that VR has an evident therapeutic effect on improving balance during the rehabilitation of children with ataxic cerebral palsy.
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.Nehad A. Abo-Zaid, Nesma A Helmy, Nader I Elsayed, Amira H Mohammed. Wii Sport versus task-oriented training on gait in unilateral cerebral palsy: A randomized controlled trial. Conference: Journal of Human Sport and Exercise. Autumn Conferences of Sports Science 2021;16.
- 2.Abo-Zaid NA, El-Gendy AM, Hewidy I, Essam Ali M, Sabbahi A. Influence of aerobic exercise on inhibitory control of executive functions in children with hemiplegic cerebral palsy: A randomized controlled trial. Clin Rehabil 2024;38:337–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37885221&dopt=Abstract 10.1177/02692155231208578 [DOI] [PubMed] [Google Scholar]
- 3.Shakiba E, Fatoorehchi S, Pishyareh E, Vahedi M, Hosseini SM. Effect of Using Wii Balance Board on Functional Balance of Children With Ataxic Cerebral Palsy. Archives of Rehabilitation. 2021;22:394–407. [Persian.] 10.32598/RJ.22.3.3289.1 [DOI] [Google Scholar]
- 4.Mitoma H, Hayashi R, Yanagisawa N, Tsukagoshi H. Gait disturbances in patients with pontine medial tegmental lesions: clinical characteristics and gait analysis. Arch Neurol 2000;57:1048–57. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10891989&dopt=Abstract 10.1001/archneur.57.7.1048 [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T, editor. Neurological Physical Therapy InTech; 2017. [Google Scholar]
- 6.Tanner L. Doctors use Wii games for rehab therapy, wii rehabilitation. The Sidney Morning Herald. February 9, 2008.
- 7.Holden MK, Dyar TA, Dayan L. Cimadoro, Telerehabilitation using a virtual environment improves upper extremity function in patients with stroke. IEEE Transactions on Neural Systems 2010. [Google Scholar]
- 8.Tarakci D, Ersoz Huseyinsinoglu B, Tarakci E, Razak Ozdincler A. Effects of Nintendo Wii-Fit® video games on balance in children with mild cerebral palsy. Pediatr Int 2016;58:1042–50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26858013&dopt=Abstract 10.1111/ped.12942 [DOI] [PubMed] [Google Scholar]
- 9.Cooper T, Williams JM. Does an exercise program integrating the Nintendo Wii-Fit Balance Board improve balance in ambulatory children with cerebral palsy? Phys Ther Rev 2017;22:229–37. 10.1080/10833196.2017.1389810 [DOI] [Google Scholar]
- 10.Tatla SK, Radomski A, Cheung J, Maron M, Jarus T. Wii-habilitation as balance therapy for children with acquired brain injury. Dev Neurorehabil 2014;17:1–15. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23231377&dopt=Abstract 10.3109/17518423.2012.740508 [DOI] [PubMed] [Google Scholar]
- 11.Rahman SA, Rahman A. Efficacy of virtual reality-based therapy on balance in children with Down syndrome. World Appl Sci J 2010;10:254–61. [Google Scholar]
- 12.de Araújo AV, Neiva JF, Monteiro CB, Magalhães FH. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. BioMed Res Int 2019;2019:7106951. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31828120&dopt=Abstract 10.1155/2019/7106951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol 2004;4:26. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15535880&dopt=Abstract 10.1186/1471-2288-4-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997;39:214–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9183258&dopt=Abstract 10.1111/j.1469-8749.1997.tb07414.x [DOI] [PubMed] [Google Scholar]
- 15.Gills S. Children with Cerebral Palsy’s Cognitive Abilities. Journal of Pediatric Neurological Disorders 2023;6:85–6. [Google Scholar]
- 16.Levitt S. Treatment of cerebral palsy and motor delay. Forth Edition. Oxford: Blackwell Scientific Publication; 2018. p. 169-223. [Google Scholar]
- 17.Elshafey MA, Abdrabo MS, Elnaggar RK. Effects of a core stability exercise program on balance and coordination in children with cerebellar ataxic cerebral palsy. J Musculoskelet Neuronal Interact 2022;22:172–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35642697&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 18.Hartley H, Cassidy E, Bunn L, Kumar R, Pizer B, Lane S, et al. Exercise and Physical Therapy Interventions for Children with Ataxia: A Systematic Review. Cerebellum 2019;18:951–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31392562&dopt=Abstract 10.1007/s12311-019-01063-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown GT, Burns SA. The efficacy of neurodevelopmental treatments in children: a systematic review. Br J Occup Ther 2001;64:235–44. 10.1177/030802260106400505 [DOI] [Google Scholar]
- 20.Kim JS. Effects of whole-body vibration exercise on functions required for bowling performance of male bowling player. J Exerc Rehabil 2019;15:78–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30899741&dopt=Abstract 10.12965/jer.1938038.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Mansec Y, Dorel S, Hug F, Jubeau M. Lower limb muscle activity during table tennis strokes. Sports Biomech 2018;17:442–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28895466&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 22.Campbell BM, Stodden DF, Nixon MK. Lower extremity muscle activation during baseball pitching. J Strength Cond Res 2010;24:964–71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20300031&dopt=Abstract 10.1519/JSC.0b013e3181cb241b [DOI] [PubMed] [Google Scholar]
- 23.Deutsch JE, Brettler A, Smith C, Welsh J, John R, Guarrera-Bowlby P, et al. Nintendo wii sports and wii fit game analysis, validation, and application to stroke rehabilitation. Top Stroke Rehabil 2011;18:701–19. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22436308&dopt=Abstract 10.1310/tsr1806-701 [DOI] [PubMed] [Google Scholar]
- 24.El-Shamy SM, Abd El Kafy EM. Effect of balance training on postural balance control and risk of fall in children with diplegic cerebral palsy. Disabil Rehabil 2014;36:1176–83. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24032716&dopt=Abstract 10.3109/09638288.2013.833312 [DOI] [PubMed] [Google Scholar]
- 25.Gstöttner M, Neher A, Scholtz A, Millonig M, Lembert S, Raschner C. Balance ability and muscle response of the preferred and nonpreferred leg in soccer players. Mot Contr 2009;13:218–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19454781&dopt=Abstract 10.1123/mcj.13.2.218 [DOI] [Google Scholar]
- 26.Arifin N, Abu Osman NA, Wan A. Interrater test-retest reliability of static and dynamic stability indexes measurement using the Biodex Stability System during unilateral stance. Appl Biomech 2014;300–4. 10.1123/jab.2013-0130 [DOI]
- 27.Abo-zaid NA. Efficacy of Lower Extremity Mirror Therapy on Balance in Children with Hemiplegic Cerebral Palsy: A Randomized Controlled Trial. Int J Psychosoc Rehabil 2020;24:8974–84. [Google Scholar]
- 28.Shousha TM, Abo-Zaid NA, Hamada HA, Abdelsamee MY, Behiry MA. Virtual reality versus Biodex training in adolescents with chronic ankle instability: a randomized controlled trial. Arch Med Sci 2021;19:1059–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37560731&dopt=Abstract 10.5114/aoms/134635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med 1995;27:27–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7792547&dopt=Abstract 10.2340/1650197719952736 [DOI] [PubMed] [Google Scholar]
- 30.Nolan L, Grigorenko A, Thorstensson A. Balance control: sex and age differences in 9- to 16-year-olds. Dev Med Child Neurol 2005;47:449–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15991864&dopt=Abstract 10.1017/S0012162205000873 [DOI] [PubMed] [Google Scholar]
- 31.Sussman M, Aiona M. Treatment of Spastic Diplegia in Patients with Cerebral Palsy. Journal of Pediatric Orthopedics. Phialdelphia, PA: Lippincott Williams & Wilkins; 2004. p. 54-9. [Google Scholar]
- 32.Ganesan M, Sathyaprabha TN, Gupta A, Pal PK. Effect of partial weight-supported treadmill gait training on balance in patients with Parkinson disease. PM R 2014;6:22–33. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24021298&dopt=Abstract 10.1016/j.pmrj.2013.08.604 [DOI] [PubMed] [Google Scholar]
- 33.Aman JE, Elangovan N, Yeh IL, Konczak J. The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci 2015;8:1075. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25674059&dopt=Abstract 10.3389/fnhum.2014.01075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Missaoui B, Thoumie P. Balance training in ataxic neuropathies. Effects on balance and gait parameters. Gait Posture 2013;38:471–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23465318&dopt=Abstract 10.1016/j.gaitpost.2013.01.017 [DOI] [PubMed] [Google Scholar]
- 35.Wolpert DM, Diedrichsen J, Flanagan JR. Principles of sensorimotor learning. Nat Rev Neurosci 2011;12:739–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22033537&dopt=Abstract 10.1038/nrn3112 [DOI] [PubMed] [Google Scholar]
- 36.Kitago T, Krakauer JW. Motor learning principles for neurorehabilitation. Handb Clin Neurol 2013;110:93–103. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23312633&dopt=Abstract 10.1016/B978-0-444-52901-5.00008-3 [DOI] [PubMed] [Google Scholar]
- 37.Keller JL, Bastian AJ. A home balance exercise program improves walking in people with cerebellar ataxia. Neurorehabil Neural Repair 2014;28:770–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24526707&dopt=Abstract 10.1177/1545968314522350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mulligan H, Mills K, Pascoe O, Smith M. Physiotherapy treatment for a child with non-progressive congenital ataxia. New Zealand J Physiotherapy. 1999;27:34–41. [Google Scholar]
- 39.Dewar R, Love S, Johnston LM. Exercise interventions improve postural control in children with cerebral palsy: a systematic review. Dev Med Child Neurol 2015;57:504–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25523410&dopt=Abstract 10.1111/dmcn.12660 [DOI] [PubMed] [Google Scholar]
- 40.White D, Burdick K, Fulk G, Searleman J, Carroll J. A virtual reality application for stroke patient rehabilitation. In: IEEE International Conference Mechatronics and Automation. Singapore; 2005. p. 1081–6. [Google Scholar]
- 41.Gatica RV, Elgueta CE, Vidal SC. Impacto del entrenamiento del balance a través de realidad virtual en una población de adultos mayores. Int J Morphol 2010;28:303–8. 10.4067/S0717-95022010000100044 [DOI] [Google Scholar]
- 42.Kwok BC, Mamun K, Chandran M, Wong CH. Evaluation of the Frails’ Fall Efficacy by Comparing Treatments (EFFECT) on reducing fall and fear of fall in moderately frail older adults: study protocol for a randomised control trial. Trials 2011;12:155. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21682909&dopt=Abstract 10.1186/1745-6215-12-155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pourazar M, Bagherzadeh F, Mirakhori F. Virtual reality training improves dynamic balance in children with cerebral palsy. Int J Dev Disabil 2019;67:429–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34925773&dopt=Abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ilg W, Schatton C, Schicks J, Giese MA, Schöls L, Synofzik M. Video game-based coordinative training improves ataxia in children with degenerative ataxia. Neurology 2012;79:2056–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23115212&dopt=Abstract 10.1212/WNL.0b013e3182749e67 [DOI] [PubMed] [Google Scholar]
- 45.Ribeiro da Silva R, Iwabe-Marchese C. Using virtual reality for motor rehabilitation in a child with ataxic cerebral palsy: case report. Fisioter Pesqui 2015;22:97–102. [Google Scholar]
- 46.Schiavinato AM, et al. Influência do Wii Fit no equilíbrio de paciente com disfunção cerebelar: estudo de caso Influence of the Wii Fit on the balance of cerebellar dysfunction patient: case study. J Health Sci Inst. 2010;28:50–2. [Google Scholar]
- 47.Staiano AE, Flynn R. Therapeutic Uses of Active Videogames: A Systematic Review. Games Health J 2014;3:351–65. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26192642&dopt=Abstract 10.1089/g4h.2013.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang M, Reid D. Virtual reality in pediatric neurorehabilitation: attention deficit hyperactivity disorder, autism and cerebral palsy. Neuroepidemiology 2011;36:2–18. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21088430&dopt=Abstract 10.1159/000320847 [DOI] [PubMed] [Google Scholar]


