Background and objectives:
In March 2020, the coronavirus disease 2019 (COVID-19) pandemic halted National Health and Nutrition Examination Survey (NHANES) field operations. As data collected in the partial 2019–2020 cycle (herein referred to as 2019–March 2020) are not nationally representative, they were combined with previously released 2017–2018 data to produce nationally representative estimates. This report explains the creation of the 2017–March 2020 prepandemic data files, provides recommendations for and limitations of the files’ use, and presents prevalence estimates for selected health outcomes based on the files.
Methods:
The 2019–2020 primary sampling units (PSUs) were reassigned to the 2015–2018 sample design strata and combined with the 2017–2018 data to create a data set that could be used to calculate nationally representative estimates. A PSU-level adjustment factor was created to equalize the contribution of each stratum to the total survey sample and applied to participant base weights. Interview and examination weights were calculated from the adjusted base weights. The performance of final interview weights was assessed by comparing the demographic characteristics of the weighted NHANES 2017–March 2020 prepandemic sample with nationally representative estimates from the 2018 5-year American Community Survey. Prevalence estimates and 95% confidence intervals were calculated for selected health outcomes.
Results:
Among children and adolescents aged 2–19 years, the prevalence of obesity was 19.7% and the prevalence of untreated or restored dental caries in one or more primary or permanent teeth was 46.0%. Among adults aged 20 and over, the age-adjusted prevalence of obesity was 41.9%, severe obesity was 9.2%, and diabetes was 14.8%. Among adults aged 18 and over, the age-adjusted prevalence of hypertension was 45.1%. Among adults aged 65 and over, the age-adjusted prevalence of complete tooth loss was 13.8%.
Conclusion:
A PSU-level adjustment factor and additional weighting adjustments made nationally representative estimates from the 2017–March 2020 prepandemic data files possible; this was the last NHANES data collected before widespread transmission of COVID-19.
Keywords:
obesity, hypertension, diabetes, tooth loss, dental cariesIntroduction
The National Health and Nutrition Examination Survey (NHANES) is unique among nationwide health surveys in the United States, combining in-person interviews with standardized physical examinations and laboratory tests. Since 1999, NHANES has operated as a continuous survey, and nationally representative data have been released in 2-year cycles (1). During March 2020, the coronavirus disease 2019 (COVID-19) pandemic halted NHANES field operations after data were only partially collected from the intended number of geographic locations in the 2019–2020 sample. As a result, analyses based solely on the partial 2019–2020 data, which are not nationally representative, would not produce results that are generalizable to the U.S. civilian noninstitutionalized population. Thus, for the first time since the initiation of the continuous NHANES in 1999, nationally representative 2-year data and estimates cannot be released. Instead, the partial 2019–2020 data (herein referred to as 2019–March 2020 data) were combined with the full data set from the previous cycle (2017–2018) to create the 2017–March 2020 prepandemic data files, which may be used to produce nationally representative estimates.
This report provides: a) a brief explanation of the creation of the NHANES 2017–March 2020 prepandemic data files; b) recommendations for analysis and limitations of these files; and c) nationally representative prevalence estimates of several selected health outcomes calculated from the files. A comprehensive National Center for Health Statistics (NCHS) Series 2 report describing the sample design, weighting methodology, response rate, and variance estimation procedures for these files will be released later in 2021. More detailed methodological reports on NHANES sample design, estimation, and analytic guidelines can be found on the NCHS website.
Overview and Description of the NHANES 2017–March 2020 Prepandemic Data Files
About NHANES
NHANES is a cross-sectional survey designed to monitor the health and nutrition of the civilian noninstitutionalized resident U.S. population. NHANES uses a complex, multistage, stratified probability sampling design. The primary sampling units (PSUs; usually a county or a group of contiguous counties) are sampled with probability proportional to size within strata (2). NHANES consists of interviews conducted in participants’ homes and in a mobile examination center (MEC) and a standardized physical examination, including tests on blood and other specimens, conducted in the MEC (1). NHANES procedures and protocols were approved by the NCHS Research Ethics Review Board. Signed informed consent was obtained from participants who had reached the age of maturity in their state (usually age 18). A parent or guardian gave permission for minors to participate. Children aged 7–17 years provided documented assent.
Creation of the 2017–March 2020 prepandemic data files
Rationale
The sample for the NHANES 2019–2020 survey cycle was selected using the 4-year 2019–2022 sample design. This design allowed each 2-year data cycle to be nationally representative and included 30 PSUs each, for a total of 60 PSUs in the 4-year 2019–2022 sample, following methods from previous sample designs (3). However, the 2019–2020 NHANES operations were suspended in mid-March 2020 due to the pandemic after data were collected in only 18 PSUs. Data collection for the remaining 12 PSUs in the cycle was canceled. Because data collection was incomplete for the full 2-year sample, the 2019–March 2020 sample is not nationally representative, and unbiased estimates cannot be produced from this partial cycle alone. To provide nationally representative estimates, the 2019–March 2020 data were combined with the previously released 2017–2018 data for content that was collected in both survey cycles and could be combined across cycles because no major changes to data collection methodology, procedures, or protocols occurred. For these combined data, additional weighting procedures were implemented to create the NHANES 2017–March 2020 prepandemic data files.
Creating a data set for nationally representative estimates
Combining NHANES 2017–2018 and 2019–March 2020 data presented statistical challenges because PSUs for these cycles were selected from different 4-year sample designs: the 2017–2018 cycle was drawn from the 2015–2018 sample design, and the 2019–2020 cycle was drawn from the 2019–2022 sample design (3). For both sample designs, the major strata, or geographical areas, used to define the first sampling stage were chosen based on urban–rural population distribution and other characteristics of the locality (3). However, because population size and other characteristics that determine major strata membership change over time, the strata comprised different PSUs in the 2015–2018 design than in the 2019–2022 design.
Because the 18 PSUs in the 2019–March 2020 sample did not represent the nation (or any defined population), the 2019–2020 PSUs were reassigned to the 2015–2018 sample design strata and combined with the 2017–2018 data to create a data set that could be used for nationally representative estimates (3). The reassignment to the 2015–2018 design ensured that the same general NHANES sampling approach used historically, including the inclusion of at least two PSUs per strata, could be maintained. The combined 2017–March 2020 prepandemic data files thus comprise a total of 48 PSUs: 30 PSUs from the 2017–2018 cycle and 18 PSUs from the 2019–March 2020 data collection, with unequal numbers of PSUs per major stratum. However, the NHANES sample design requires equal numbers of PSUs per major stratum; therefore, special weighting measures were needed to calibrate the data set back to an equal number of PSUs across major strata.
Weighting procedures
A PSU-level adjustment factor was created to equalize the contribution of each stratum to the total survey sample and applied to participant base weights. This approach is similar to an approach that could have been taken to combine a probability sample with a nonprobability sample, modeling the contribution of the 2019–2020 data based on the 2015–2018 stratification. In this application, the fact that the 2019–2020 PSUs were a subset of a probability sample adds credibility to the approach. The PSU-level adjustment was derived to effectively increase the weights from underrepresented strata and reduce the weights from overrepresented strata, while improving the efficiency of the combined sample (4). Interview weights and MEC weights then were calculated using standard methodology including adjusting for nonresponse and unequal probability of selection and calibrating to known population totals (2,3).
The performance of interview weights was assessed by comparing the demographic characteristics of the weighted NHANES 2017–March 2020 prepandemic sample with nationally representative estimates from the 2018 5-year American Community Survey (ACS) (5). The 2018 5-year ACS and NHANES 2017–March 2020 prepandemic estimates were consistent for adult education, marital status, household composition, and health insurance coverage (comparisons used the same methodology used to compare 2017–2018 NHANES estimates with ACS estimates) (2). However, a statistically significant difference in urban–rural distribution between NHANES and ACS was seen across four categories: large central, large fringe, medium and small metropolitan areas, and micropolitan and noncore. The weights were recalibrated to NCHS rural–urban code categories in addition to the three dimensions used for the NHANES 2017–2018 weighting calibration (race–Hispanic origin–age–sex demographic subgroups, race–Hispanic origin–sex–education level subgroups, and area-level household income) (3). The introduction of the additional dimension resulted in the weighted 2017–March 2020 sample being more consistent with the urban–rural distribution of the 2018 5-year ACS file than previously, with no statistically significant differences between NHANES and ACS in the proportion of sample in each urban–rural designation category. The weights are designed to yield nationally representative estimates for the entire period covered by the 2017–March 2020 prepandemic data files.
Other considerations
While the 2017–March 2020 prepandemic data files generally provide prevalence estimates similar to those of the 2017–2018 files, the decreased variance and increased sample size allow more reliable comparison of statistical differences between subgroups. As for all analyses using NHANES data, the complex survey design should be taken into account for estimation of variance (6).
Comparisons or examination of trends between 2017–2018 and 2019–March 2020 data are not possible and should not be conducted because the 2019–March 2020 data do not represent any defined population. To prevent data analysts from separating the two cycles, changes have been made to respondent sequence identification numbers, and PSU and strata variables have been masked. Additionally, there are no appropriate survey weights to make national estimates using 2019–March 2020 data.
Due to the unusual circumstances surrounding the construction of this file and the need to reduce disclosure risk for participants in the partially completed cycle, the 2017–March 2020 prepandemic data release is more limited in content compared with previous 2-year files. Currently available data files are presented in Table 1. Additional files may be released to the public in the future. Other 2017–March 2020 prepandemic data files will also be released through the NCHS Research Data Center, including data determined to have disclosure risks that require additional measures to protect confidentiality (7). Data on indicators that were collected only during 2019–March 2020 will be released as a convenience sample through the NCHS Research Data Center (7).
Table 1
Data files included in the initial public release of the National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files
Prevalence Estimates of Selected Health Outcomes From the NHANES 2017–March 2020 Prepandemic Data Files
Health outcomes selected for presentation in this report include obesity and dental caries (untreated or restored) among children and adolescents; obesity, severe obesity, hypertension, and diabetes among adults; and complete tooth loss among older adults.
Methodology to calculate 2017–March 2020 prepandemic health outcome prevalence estimates
Definitions of health outcomes
For hypertension, a new methodology for measuring blood pressure (BP), an oscillometric protocol (OP), was introduced during the 2017–2018 cycle, concurrently with the auscultatory protocol (AP), used historically in NHANES, and was used exclusively during 2019–March 2020 data collection. During 2017–2018, both OP and AP were performed; however, previously released 2017–2018 estimates used the AP method (8,9). BP measurements released within the 2017–March 2020 prepandemic data files reflect use of the OP method. For the new OP method, BP was measured in the MEC by health technicians using a standard methodology with an automatic oscillometric BP device (10,11). While an investigation contrasting the AP and OP approach in the same subjects during survey years 2017–2018 showed some between-protocol differences, stage I hypertension estimates generally agreed (11).
The remaining health outcomes have been reported for previous NHANES data releases and are defined similarly here (12–17). Definitions of all outcomes are included in the Technical Notes. The methodology used to obtain these measurements can be found on the NHANES website (18–23). Measurements of all reported health outcomes presented in this report were collected using the same protocols during 2017–2018 and 2019–March 2020.
Definitions of covariates
Prevalence estimates were calculated by sex, age category, race and Hispanic origin, family income, and, for some health outcomes, education and weight status. To provide consistency with previously reported estimates from NHANES, age categories were defined specifically for each health outcome. Definitions for covariates are included in the Technical Notes.
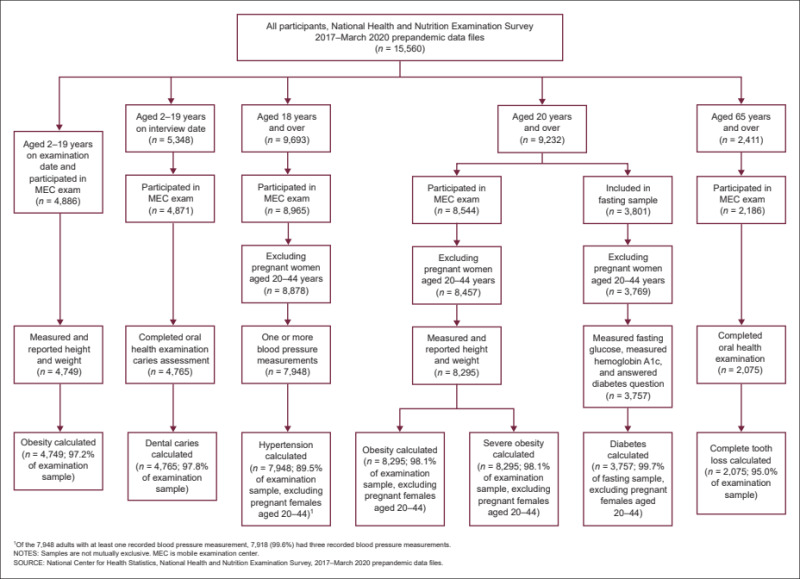
Description of included sample
The original survey design for the 2017–2018 cycle (the 2015–2018 design) and the 2019–2020 cycle (the 2019–2022 design) used oversampling to improve the reliability of estimates among several subgroups including: Hispanic persons, non-Hispanic black persons, non-Hispanic and non-black Asian persons, non-Hispanic white persons and persons of other races and ethnicities at or below 185% of the federal poverty level (FPL), and non-Hispanic white persons and persons of other races and ethnicities aged 0–11 years or 80 and over (3). All pregnant females were excluded from the analyses for obesity and severe obesity. Pregnant women aged 20–44 were excluded from the analyses for hypertension and diabetes. Pregnant women outside of this age range were not excluded from the analyses for hypertension and diabetes because pregnancy status is not reported due to disclosure concerns. Inclusion criteria and sample sizes for each health outcome are defined in the Figure. Unweighted NHANES examination response rates during 2017–March 2020 were 51.4% for children and adolescents aged 2–19 years and 43.9% for adults aged 20 and over.
To provide a comparison of sample size and variance, overall estimates for each health outcome were also calculated for the 2017–2018 survey cycle alone using the same methodology. Some of these estimates have previously been reported elsewhere (14,15,17).
Statistical methods
Sample weights were used for all analyses and accounted for unequal probability of selection, were adjusted for nonresponse, and were calibrated to known population totals as described previously (2,3). Examination sample weights were used for all outcomes except total diabetes, for which morning fasting sample weights were used. All analyses accounted for the survey’s complex, multistage probability design. For adults, prevalence estimates were age adjusted to the 2000 projected U.S. Census population using the direct method (24). Standard errors were estimated using Taylor series linearization, and 95% confidence intervals were calculated using the methodology proposed by Korn and Graubard (25). The reliability of estimates was assessed using the “National Center for Health Statistics data presentation standards for proportions” (26). Estimates that did not meet these standards are noted. Significance testing for pairwise differences between groups within unordered covariates was performed using a two-sided univariate t statistic. For ordered covariates with an apparent monotonic pattern, linear trends across groups were tested using orthogonal contrast matrices. For ordered covariates with no apparent monotonic pattern, pairwise differences were tested between groups using a two-sided univariate t statistic. All reported differences and trends were statistically significant (p < 0.05) unless otherwise indicated. All analyses were performed using R (R Foundation for Statistical Computing), including the R survey package, SAS version 9.4 (SAS Institute, Inc., Cary, N.C.), or SUDAAN version 11.0 (RTI International, Research Triangle Park, N.C.) (27).
Results for 2017–March 2020 prepandemic health outcome estimates
Overall estimates
Among children and adolescents aged 2–19 years, the prevalence of obesity during 2017–March 2020 was 19.7% (95% confidence interval [CI]: 17.9–21.6) and the prevalence of dental caries (untreated or restored) was 46.0% (95% CI: 42.9–49.1; Table 2). Among adults aged 20 and over, the age-adjusted prevalence of obesity was 41.9% (95% CI: 39.4–44.3), the age-adjusted prevalence of severe obesity was 9.2% (95% CI: 8.0–10.6), and the age-adjusted prevalence of diabetes was 14.8% (95% CI: 13.1–16.7; Table 2). Among adults aged 18 and over, the age-adjusted prevalence of hypertension was 45.1% (95% CI: 42.5–47.6; Table 2). Among adults aged 65 and over, the age-adjusted prevalence of complete tooth loss was 13.8% (95% CI: 10.6–17.6; Table 2). Estimates for 2017–2018 are included for reference; however, statistical testing for comparison to 2017–March 2020 cannot be performed because the samples are not independent (Table 2). Generally, estimates from 2017–March 2020 were similar to those from 2017–2018, and the standard errors were similar or smaller.
Obesity among children and adolescents
Among all children and adolescents aged 2–19 years, obesity prevalence increased with age (12.7% for those aged 2–5 years, 20.7% for 6–11, and 22.2% for 12–19), was highest among Hispanic (26.2%) and non-Hispanic black (24.8%) children and adolescents, followed by non-Hispanic white (16.6%) and non-Hispanic Asian (9.0%) children and adolescents, and decreased with increasing family income (Table 3). Prevalence of obesity among children and adolescents aged 2–19 years was similar among boys and girls (20.9% compared with 18.5%). Boys had a higher prevalence of obesity than girls among those aged 6–11 years, among non-Hispanic Asian children and adolescents, and among those with family income more than 350% FPL. However, among non-Hispanic black children and adolescents, obesity prevalence was lower among boys compared with girls. A few differences in the patterns of obesity by sociodemographic characteristics between boys and girls were seen. For boys, obesity prevalence was higher among those aged 6–11 and those aged 12–19 years than among those aged 2–5 years, whereas obesity increased with increasing age among girls. Also among boys, obesity prevalence was highest among Hispanic boys compared with other race and Hispanic-origin groups. Among girls, obesity prevalence was significantly different between each race and Hispanic origin-group, with the highest prevalence among non-Hispanic black girls. The prevalence of obesity decreased with increasing family income for both boys and girls.
Table 3
Prevalence of children and adolescents aged 2–19 years with obesity, by demographic characteristics: United States, 2017–March 2020
Untreated or restored dental caries among children and adolescents
For all children, the prevalence of dental caries (untreated or restored) was highest among Hispanic children and adolescents (Hispanic: 54.5%, non-Hispanic Asian: 46.6%, non-Hispanic white: 42.7%, and non-Hispanic black: 41.7%; Table 4). Prevalence of dental caries increased with age among children and adolescents overall (22.0% for those aged 2–5 years, 48.1% for 6–11, and 56.0% for 12–19), but decreased with family income (130% or less FPL: 53.5%, more than 130% through 350% FPL: 47.4%, and more than 350% FPL: 35.8%). Prevalence of any dental caries was similar among both boys and girls overall (47.5% compared with 44.5%) but was higher among boys for those aged 6–11 years. Among both boys and girls, prevalence of dental caries increased with age and decreased with increasing family income. The prevalence of dental caries was higher among Hispanic boys than non-Hispanic black boys and was higher among Hispanic girls than non-Hispanic white and non-Hispanic black girls.
Table 4
Prevalence of children and adolescents aged 2–19 years with untreated or restored dental caries, by demographic characteristics: United States, 2017–March 2020
Obesity among adults
No differences in obesity prevalence were seen with age (39.8% for those aged 20–39, 44.3% for 40–59, and 41.5% for 60 and over) among all adults (Table 5). Obesity was most common among non-Hispanic black adults (non-Hispanic black: 49.9%, Hispanic: 45.6%, non-Hispanic white: 41.4%, and non-Hispanic Asian: 16.1%). Obesity prevalence was lower among adults with family income of more than 350% FPL (39.0%) compared with those with family income more than 130% through 350% FPL (46.5%) but was not different than those with family income 130% or less FPL (43.9%). Obesity was also highest among those with a high school diploma or some college (46.4%) followed by those with less than a high school diploma (40.1%) and those with a college degree or above (34.2%). No differences in obesity prevalence were observed between men and women overall (41.8% each, Table 5). However, a higher percentage of women than men had obesity among non-Hispanic black adults, adults with family income of 130% or less FPL, and adults with less than a high school diploma. Patterns of obesity among adults differed according to some characteristics by sex. There was a higher percentage of men aged 40–59 than men aged 60 and over with obesity, while obesity was not associated with age among women. Non-Hispanic black women had the highest prevalence of obesity compared with women of other race and Hispanic-origin groups. Among men, obesity prevalence was lowest among non-Hispanic Asian men but did not differ between other race and Hispanic-origin groups. Although no differences were seen in obesity by family income categories among men, obesity was lowest among women with family income more than 350% FPL. Patterns of obesity prevalence by education were different for men than for women. Among men, prevalence was highest among those with a high school diploma or some college, while among women, prevalence was higher for those with less than a high school diploma and those with a high school diploma or some college compared with those with a college degree or above.
Table 5
Prevalence of adults aged 20 and over with obesity, by demographic characteristics: United States, 2017–March 2020
Severe obesity among adults
The prevalence of severe obesity was lowest among those aged 60 and over (9.7% for those aged 20–39, 10.7% for 40–59, and 6.1% for 60 and over; Table 6). For men and women combined, all groups were different from each other except non-Hispanic white and Hispanic adults (non-Hispanic black: 14.0%, non-Hispanic white: 9.5%, Hispanic: 7.4%, and non-Hispanic Asian: 1.8%). Those with family income of more than 350% FPL had the lowest prevalence of severe obesity (130% or less FPL: 10.9%, more than 130% through 350% FPL: 11.8%, and more than 350% FPL: 6.9%) and those with a high school diploma or some college had a higher prevalence (11.3%) of severe obesity than those with less than a high school diploma (7.6%) and those with a college degree or above (6.1%). A higher percentage of women than men had severe obesity overall (11.7% compared with 6.6%; Table 6) and among every age, race and Hispanic origin, family income, and education category, with the exceptions of non-Hispanic Asian and Hispanic adults, no differences were seen. Among men, non-Hispanic Asian men had a lower prevalence of severe obesity than other race and Hispanic-origin groups. Among women, the prevalence of severe obesity differed between all race and Hispanic-origin groups, with the highest among non-Hispanic black women and the lowest among non-Hispanic Asian women. The prevalence of severe obesity was higher in men with family income more than 130% through 350% FPL than those with family income more than 350% FPL but not those with family income 130% or less FPL, and was highest among those with a high school diploma or some college. Among women, the prevalence of severe obesity was lowest among those with family income more than 350% FPL and was lower in those with a college degree or above than among those with a high school diploma or some college.
Table 6
Prevalence of adults aged 20 and over with severe obesity, by demographic characteristics: United States, 2017–March 2020
Hypertension among adults
Hypertension prevalence increased with age among all adults (23.4% for those aged 18–39, 52.4% for 40–59, and 74.1% for 60 and over), and was highest among non-Hispanic black adults for men and women combined (non-Hispanic black: 56.9%, non-Hispanic white: 43.5%, non-Hispanic Asian: 44.6%, and Hispanic: 42.7%; Table 7). The prevalence of hypertension was lower among those with family income more than 350% FPL compared with those with family income more than 130% through 350% FPL and was lowest among those with a college degree or above. Hypertension prevalence also increased with weight status (normal weight: 31.1%, overweight: 40.6%, and obesity: 57.7%). The prevalence of hypertension was higher among men than women overall (48.7% compared with 41.2%). Prevalence of hypertension was also higher for men than women among the following subgroups: age groups 18–39 and 40–59, non-Hispanic Asian, Hispanic, family income more than 130% through 350% and more than 350% FPL, high school diploma or some college, college degree or above, those with normal weight status, and those with overweight status. Prevalence of hypertension increased among both men and women with age and with weight status. Among men, hypertension prevalence was lower for those with a college degree or above compared with those with a high school diploma or some college, whereas among women, hypertension prevalence decreased with increasing education levels. No association between hypertension prevalence and family income among men was seen; the prevalence of hypertension decreased with increasing family income among women. Prevalence of hypertension was higher among non-Hispanic black women and non-Hispanic black men than other race and Hispanic-origin groups.
Table 7
Prevalence of adults aged 18 and over with hypertension, by demographic characteristics: United States, 2017–March 2020
Diabetes among adults
Diabetes prevalence increased with age (4.4% for those aged 20–39, 16.4% for 40–59, and 30.0% for 60 and over) among all adults (Table 8). Non-Hispanic white adults had a lower prevalence of diabetes (12.0%) than other race and Hispanic-origin groups (Hispanic: 21.2%, non-Hispanic black: 18.8%, non-Hispanic Asian: 18.1%). For men and women combined, the prevalence of diabetes decreased with increasing family income (130% or less FPL: 20.0%, more than 130% through 350% FPL: 17.7%, and more than 350% FPL: 10.9%) and educational attainment (less than high school diploma: 22.7%, high school diploma or some college: 15.7%, and college degree or above: 10.4%) and increased with increasing weight status (normal weight: 6.6%, overweight: 10.3%, obesity: 23.3%). Men had a higher prevalence of diabetes than women overall (16.3% compared with 13.4%) as well as among those aged 60 and over, those with family income more than 350% FPL, those with a college degree or above, and those in the overweight category. The patterns of diabetes prevalence by age, race and Hispanic origin, family income, educational attainment, and weight status among both men and women followed the same patterns seen among all adults.
Table 8
Prevalence of adults aged 20 and over with diabetes, by demographic characteristics: United States, 2017–March 2020
Complete tooth loss among older adults
The prevalence of complete tooth loss increased with age among all adults (10.6% for those aged 65–69, 10.8% for 70–74, and 17.3% for 75 and over) and was higher in non-Hispanic black (21.0%) than non-Hispanic white (12.3%) adults, but otherwise did not differ by race and Hispanic origin (Table 9). Complete tooth loss decreased with increasing family income and increasing education (less than high school diploma: 31.5%, high school diploma or some college: 15.0%, and college degree or above: 2.7%). The prevalence of complete tooth loss did not vary between men and women (14.0% compared with 13.6%) overall; however, among those with family income more than 130% through 350% FPL, men had a higher prevalence of complete tooth loss than women. Among men, complete tooth loss was higher in non-Hispanic black than non-Hispanic white and non-Hispanic Asian adults. The prevalence of complete tooth loss decreased with increasing family income and with increasing educational attainment among both men and women.
Table 9
Prevalence of adults aged 65 and over with complete tooth loss, by demographic characteristics: United States, 2017–March 2020
Discussion
The COVID-19 pandemic led to an unprecedented disruption of NHANES operations. While the data collected for the planned 2019–2020 NHANES cycle cannot be released in their usual 2-year format, methodological procedures were implemented to produce files that could provide updated nationally representative estimates by combining the available 2019–March 2020 data with existing 2017–2018 data.
Estimates for health outcomes calculated from the 2017–March 2020 prepandemic data files presented here are similar to 2017–2018 estimates. This reflects both the methodological adjustments as well as the patterns in prevalence estimates that typically are not expected to vary greatly annually in NHANES due to the relatively small sample size in a 1-year data collection. Data collected in 2019 make up the majority of the 2019–March 2020 data. The 2017–March 2020 prepandemic estimates and 2017–2018 estimates for the overall population fall well within each other’s 95% confidence intervals. However, because the samples are not independent, statistical testing comparing these time periods cannot be performed and any differences should not be interpreted as a possible trend between 2017–2018 and 2019–March 2020. Besides inclusion of the most recently collected NHANES data, one potential benefit of data from the 2017–March 2020 prepandemic data files is the larger sample size, which may be beneficial when performing analyses with smaller subgroups. For the most part, this increased sample size leads to improved precision and smaller variance estimates. For example, the standard error for prevalence estimates for childhood obesity, childhood dental caries, adult obesity, adult severe obesity, adult hypertension, and adult diabetes are all lower in the 2017–March 2020 prepandemic estimates than the 2017–2018 estimates. However, for some estimates and some demographic subgroups, increased variation in the sampling weights, increased variation in the true underlying population values of the health outcomes from the data added from 2019–March 2020, or both may result in equivalent or increased variance of estimates. For example, the standard error for complete tooth loss among older adults is the same in 2017–March 2020 prepandemic estimates as in 2017–2018 estimates.
The 2017–March 2020 prepandemic data files are subject to several limitations that should be considered during analysis and when interpreting results. First, response rates on national surveys, including NHANES, have declined over the past two decades. A nonresponse bias study published on the previously released NHANES 2017–2018 data showed that the weighting methodology used for prior survey cycles was insufficient to account for nonresponse and sampling variability bias, but that enhanced weighting adjustments for education and income helped mitigate bias (2). Those weighting adjustments were also applied to the 2017–March 2020 data after the PSU-level adjustments were made, and an additional adjustment for urban–rural designation was also included. Second, the PSU-level adjustments to survey weights to account for the reassignment of 2019–March 2020 PSUs to the 2015–2018 sample design were designed for overall estimates and not specific subgroups. Therefore, any trend comparisons over time for subgroups (e.g., by age, sex, race and Hispanic origin) between the 2017–March 2020 prepandemic data files and previous NHANES cycles should be interpreted in this context and with caution. The magnitude and direction of the trend within a certain subgroup may vary from the overall trend. In conducting analyses and interpreting results, analysts should consider the historical context of the trends in addition to the methodological approach to create the 2017–March 2020 prepandemic data files. Further, the unequal spacing of the 2017–March 2020 time period in relation to other NHANES cycles should be taken into account (28).
Conclusion
The halting of NHANES field operations in March 2020 due to the COVID-19 pandemic prevented collection of a nationally representative sample during the planned 2019–2020 data cycle. To obtain nationally representative estimates, the 2017–2018 cycle and the partially completed 2019–2020 cycle were combined into the NHANES 2017–March 2020 prepandemic data files, and adjustments were made to account for the incomplete PSU collection. These files contain the last NHANES data collected before widespread transmission of COVID-19. As shown in the selected estimates reported here, the 2017–March 2020 prepandemic data files produce estimates similar to the previously released NHANES data files from 2017–2018 but provide a larger sample size and more precise estimates for most of the health conditions examined in this report.
Acknowledgments
This report was prepared in the Division of Health and Nutrition Examination Surveys under the general direction of Ryne Paulose-Ram, Acting Director. The authors would like to acknowledge the assistance of Cynthia L. Ogden in the concept development of this report, Amy M. Branum and Namanjeet Ahluwalia for valuable comments in writing this report, Tala H.I. Fakhouri, Ryne Paulose-Ram, Jason Clark, and Leyla K. Mohadjer in the development of the data files used in this report, and the National Center for Health Statistics Board of Scientific Counselors for their advice and recommendations in the creation of the data files used in this report.
References
- 1.
- Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National Health and Nutrition Examination Survey: Plan and operations, 1999–2010. National Center for Health Statistics. Vital Health Stat 1(56). 2013.
- 2.
- Fakhouri THI, Martin CB, Chen TC, Akinbami LJ, Ogden CL, Paulose-Ram R, et al. An investigation of nonresponse bias and survey location variability in the 2017–2018 National Health and Nutrition Examination Survey. National Center for Health Statistics. Vital Health Stat 2(185). 2020.
- 3.
- Chen TC, Clark J, Riddles MK, Mohadjer LK, Fakhouri THI. National Health and Nutrition Examination Survey, 2015−2018: Sample design and estimation procedures. National Center for Health Statistics. Vital Health Stat 2(184). 2020.
- 4.
- Krenzke T, Mohadjer L. Application of probability-based link-tracing and nonprobability approaches to sampling out-of-school youth in developing countries. J Surv Stat Methodol. 2020.
- 5.
- U.S. Census Bureau. 2018 5-Year American Community Survey (ACS). 2019. Available from: https://www
.census.gov /programs-surveys/acs. - 6.
- Division of Health and Nutrition Examination Surveys. National Health and Nutrition Examination Survey: Analytic guidelines, 2011–2014 and 2015–2016. National Center for Health Statistics. 2018.
- 7.
- National Center for Health Statistics. Research Data Center: Restricted data. 2019. Available from: https://www
.cdc.gov/rdc /b1datatype/dt100.htm. - 8.
- Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017–2018. NCHS Data Brief, no 364. Hyattsville, MD: National Center for Health Statistics. 2020.
- 9.
- National Center for Health Statistics. National Health and Nutrition Examination Survey: 2017–2018 data documentation, codebook, and frequencies: Blood pressure. 2020. Available from: https://wwwn
.cdc.gov /Nchs/Nhanes/2017-2018/BPX_J.htm. - 10.
- National Center for Health Statistics. National Health and Nutrition Examination Survey: Blood pressure procedures manual. 2019. Available from: https://wwwn
.cdc.gov /nchs/data/nhanes/2019-2020 /manuals/2019-Blood-Pressure-Procedures-Manual-508 .pdf. - 11.
- Ostchega Y, Nwankwo T, Chiappa M, Wolz M, Graber J, Nguyen DT. Comparing blood pressure values obtained by two different protocols: National Health and Nutrition Examination Survey, 2017–2018. National Center for Health Statistics. Vital Health Stat 2(187). 2021.
- 12.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2020. Diabetes Care 43(Suppl 1):S14–S31. 2020.
- 13.
- Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015–2016. NCHS Data Brief, no 307. Hyattsville, MD: National Center for Health Statistics. 2018.
- 14.
- Fleming E, Afful J, Griffin SO. Prevalence of tooth loss among older adults: United States, 2015–2018. NCHS Data Brief, no 368. Hyattsville, MD: National Center for Health Statistics. 2020.
- 15.
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020.
- 16.
- Mendola ND, Chen T-C, Gu Q, Eberhardt MS, Saydah S. Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016. NCHS Data Brief, no 319. Hyattsville, MD: National Center for Health Statistics. 2018.
- 17.
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020.
- 18.
- National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES): Anthropometry procedures manual. 2017. Available from: https://wwwn
.cdc.gov /nchs/data/nhanes/2017-2018 /manuals/2017 _Anthropometry_Procedures_Manual.pdf. - 19.
- National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES): MEC laboratory procedures manual. 2017. Available from: https://wwwn
.cdc.gov /nchs/data/nhanes/2017-2018 /manuals/2017 _MEC_Laboratory_Procedures_Manual.pdf. - 20.
- National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES): Oral health examiners manual. 2018. Available from: https://wwwn
.cdc.gov /nchs/data/nhanes/2017-2018 /manuals/2018 _Oral_Health_Examiners_Manual.pdf. - 21.
- National Center for Health Statistics. National Health and Nutrition Examination Survey, 2017–2018 data documentation, codebook, and frequencies: Plasma fasting glucose. 2020. Available from: https://wwwn
.cdc.gov /Nchs/Nhanes/2017-2018/GLU_J.htm. - 22.
- National Center for Health Statistics. National Health and Nutrition Examination Survey, 2017–2018 data documentation, codebook, and frequencies: Glycohemoglobin. 2020. Available from: https://wwwn
.cdc.gov /Nchs/Nhanes/2017-2018/GHB_J.htm. - 23.
- National Center for Health Statistics. National Health and Nutrition Examination Survey, 2017–2018 data documentation, codebook, and frequencies: Diabetes. 2020. Available from: https://wwwn
.cdc.gov /Nchs/Nhanes/2017-2018/DIQ_J.htm. - 24.
- Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People Statistical Notes, no 20. Hyattsville, MD: National Center for Health Statistics. 2001.
- 25.
- Korn EL, Graubard BI. Confidence intervals for proportions with small expected number of positive counts estimated from survey data. Surv Methodol 24(2):193–201. 1998.
- 26.
- Parker JD, Talih M, Malec DJ, Beresovsky V, Carroll M, Gonzalez JF, et al. National Center for Health Statistics data presentation standards for proportions. National Center for Health Statistics. Vital Health Stat 2(175). 2017.
- 27.
- Lumley T. Survey: Analysis of complex survey samples (R package version 3.36 ed) [computer software]. 2019.
- 28.
- Ingram DD, Malec DJ, Makuc DM, Kruszon-Moran D, Gindi RM, Albert M, et al. National Center for Health Statistics guidelines for analysis of trends. National Center for Health Statistics. Vital Health Stat 2(179). 2018.
Technical Notes
Definitions of health outcomes
Body mass index, obesity, and severe obesity
Height and weight were measured using a standard protocol. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared, rounded to one decimal place. Obesity in adults aged 20 and over was defined as a BMI of greater than or equal to 30 kg/m2, while severe obesity was defined as a BMI of greater than or equal to 40 kg/m2. Obesity in children and adolescents aged 2–19 years was defined as a BMI of greater than or equal to the age- and sex-specific 95th percentile of the 2000 Centers for Disease Control and Prevention Clinical Growth Charts. Although these definitions of obesity and severe obesity are based on BMI, this is not a direct measure of body fat. Body composition varies by sex, age, and race and Hispanic origin and affects the relationship between BMI and body fat. Health risks may vary among different groups at the same BMI.
Hypertension
All blood pressure (BP) readings were obtained during a single examination. After a 5-minute rest in a seated position, participants had up to three brachial systolic and diastolic BP measurements taken 1 minute apart. An average of up to three systolic and diastolic BP readings were used for systolic and diastolic BP values. During the in-home interview, participants were asked whether they currently take a medication to lower high BP. Criteria from the American College of Cardiology and the American Heart Association were used to define hypertension. Hypertension was defined here as a measured systolic BP greater than or equal to 130 mm Hg, a measured diastolic BP greater than or equal to 80 mm Hg, or currently taking a medication to lower high BP.
Diabetes
During the in-home interview, participants were asked “Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” Participants were randomly assigned to a morning, afternoon, or evening examination. Fasting plasma glucose (from those assigned to the morning examination, after an 8- to 24-hour fast) and hemoglobin A1c were measured from venous blood samples, collected in the mobile examination center (MEC) from participants using standardized protocols. Plasma fasting glucose values reported in 2017–March 2020 prepandemic data were already adjusted using a forward regression equation for comparability as described in the data documentation. Criteria from the American Diabetes Association were used to define diabetes. Diabetes was defined here as those who had at least one of the following: a) answered “yes” to the question about being told that they have diabetes, b) had a fasting plasma glucose greater than or equal to 126 mg/dL, or c) had a hemoglobin A1c greater than or equal to 6.5%. This definition includes both those with previously diagnosed diabetes and undiagnosed diabetes. Two participants who did not answer the interview question about having diabetes and 10 participants who did not have hemoglobin A1c values were excluded.
Dental caries and complete tooth loss
The National Health and Nutrition Examination Survey (NHANES) includes an oral health examination in the MEC. Trained, licensed dentists conduct the oral health examination. Among the components of this examination were a tooth count assessment and a comprehensive dental surface-by-dental surface evaluation. During the tooth count assessment, the presence of a tooth, whether it was a permanent or primary tooth, and if the root tip was present were noted. During the dental surface-by-dental surface evaluation, the presence of untreated caries and dental restorations was assessed. The presence of dental caries is defined as having untreated or restored dental caries in one or more primary or permanent teeth. Missing teeth due to dental disease are not included in this definition. Complete tooth loss in adults is defined here as having no natural tooth, no dental root fragment, and no implanted tooth present. Measures for permanent teeth were based on 28 teeth, excluding third molars.
Definitions of covariates
Age
For childhood and adolescent obesity and dental caries, age categories were defined as 2–5, 6–11, and 12–19 years. For adult obesity, severe obesity, and diabetes, age categories were defined as 20–39, 40–59, and 60 and over. For adult hypertension, age categories were defined as 18–39, 40–59, and 60 and over. For tooth loss in older adults, age categories were defined as 65–69, 70–74, and 75 and over. For childhood obesity, age was defined using age at the time of examination (this age information is not available in publicly released data files to protect participant confidentiality). For all other health outcomes, age was defined using age at interview. For adults and older adults, these same age groupings were used for age adjustment.
Race and Hispanic origin
Race and Hispanic origin were categorized as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, and Hispanic. Participants who were categorized as other race, including multiracial, were included in total estimates but are not shown separately.
Family income
Family income was defined as the percentage of family income relative to the federal poverty level (FPL), which accounts for inflation, family size, and geographic location. Categories were 130% or less, more than 130% through 350%, and more than 350% of the FPL.
Education
Education was defined for adults aged 20 and over as the highest degree or grade finished. Categories were defined as: a) less than high school diploma, b) high school diploma or equivalent, associate’s degree, or some college, and c) college degree or above. Information on education of those under age 20 is not available publicly in this data set, given concerns for disclosure risk. Those under 20 were not included in estimates by education.
Weight status
Weight status categories were used as covariates for some outcomes and defined for adults as normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), and obesity (BMI 30.0 kg/m2 and higher).
National Center for Health Statistics
Brian C. Moyer, Ph.D., Director
Amy M. Branum, Ph.D., Acting Associate Director for Science
Division of Health and Nutrition Examination Surveys
Ryne Paulose-Ram, M.A., Ph.D., Acting Director
Namanjeet Ahluwalia, Ph.D., D.Sc., Acting Associate Director for Science
For e-mail updates on NCHS publication releases, subscribe online at: https://www.cdc.gov/nchs/email-updates.htm.
For questions or general information about NCHS: Tel: 1–800–CDC–INFO (1–800–232–4636) • TTY: 1–888–232–6348
Internet: https://www.cdc.gov/nchs • Online request form: https://www.cdc.gov/info • CS324470
- Stierman B, Afful J, Carroll MD, Chen TC, Davy O, Fink S, et al. National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files—Development of files and prevalence estimates for selected health outcomes. National Health Statistics Reports; no 158. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: https://dx.doi.org/10.15620/cdc:106273. [PMC free article]
Publication Details
Author Information and Affiliations
Authors
Bryan Stierman, M.D., M.P.H., Joseph Afful, M.S., Margaret D. Carroll, M.S.P.H., Te-Ching Chen, Ph.D., Orlando Davy, M.P.H., Steven Fink, M.A., Cheryl D. Fryar, M.S.P.H., Qiuping Gu, Ph.D., Craig M. Hales, M.D., M.P.H., Jeffery P. Hughes, M.P.H., Yechiam Ostchega, Ph.D., R.N., Renee J. Storandt, M.T.(A.S.C.P.), M.S.P.H., and Lara J. Akinbami, M.D.Publication History
Published online: June 14, 2021.
Copyright
Publisher
National Center for Health Statistics (US), Hyattsville (MD)
NLM Citation
Stierman B, Afful J, Carroll MD, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files—Development of Files and Prevalence Estimates for Selected Health Outcomes. 2021 Jun 14. In: National Health Statistics Reports [Internet]. Hyattsville (MD): National Center for Health Statistics (US); 2024 Jul-. Number 158. doi: 10.15620/cdc:106273